Empyema refers to a suppurative infection characterized by the accumulation of purulent exudate in the pleural cavity. Based on pathological progression, empyema can be classified into acute and chronic stages; based on the causative pathogens, it can be classified as pyogenic, tuberculous, or caused by specific pathogens; and based on the extent of involvement, it can be categorized as total empyema or localized empyema.
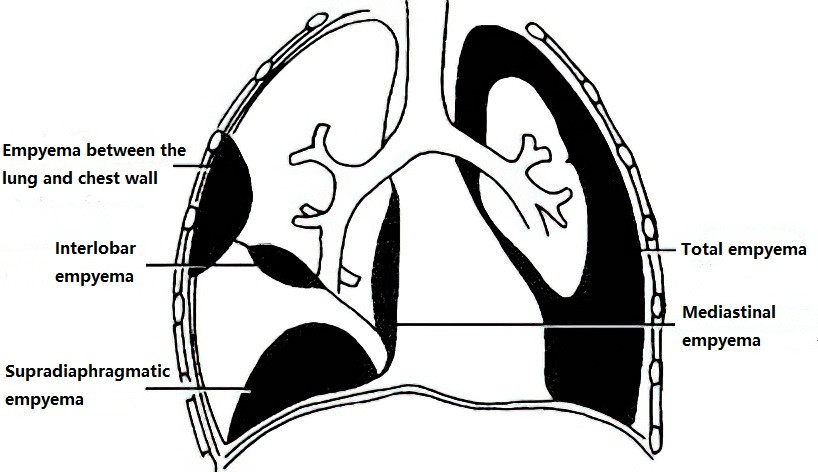
Figure 1 Classification of empyema (Illustration)
Etiology and Pathology
The causative bacteria of empyema often originate directly from pulmonary infections, though in some cases they may come from other thoracic or mediastinal organ abnormalities, such as trauma, contamination of the pleural cavity during surgery, rupture of thoracic hollow organ structures, or as complications from procedures like bronchopleural fistulas. In some instances, infections may originate from foci in other parts of the body that invade the pleural cavity directly or via lymphatic spread, such as subdiaphragmatic abscesses, liver abscesses, mediastinal abscesses, or purulent pericarditis, resulting in a pyogenic infection. Cases secondary to septicemia or bacteremia are typically caused by hematogenous dissemination. Common pathogens include Streptococcus pneumoniae and Streptococcus spp., though their frequency has declined with widespread antibiotic use. Conversely, infections caused by Staphylococcus aureus, especially drug-resistant Staphylococcus aureus, have markedly increased, particularly among pediatric patients, and are more challenging to manage. Additional commonly encountered pathogens include Escherichia coli, Pseudomonas aeruginosa, and fungi, which, though less common, are becoming increasingly significant. Anaerobic bacterial infections may lead to putrid or necrotizing empyema.
The disease progression of empyema occurs in a gradual manner and can be divided into three stages. From a clinical perspective, the first and second stages are referred to as acute empyema, while the third stage is classified as chronic empyema:
Stage 1 (Parapneumonic Effusion Phase)
Following pleural involvement by infection, extensive pleural effusion occurs. In the early phase, the pus remains thin and can flow freely within the pleural cavity. The characteristics of the pleural fluid include a serous nature, low white blood cell count, lactate dehydrogenase (LDH) levels lower than half of serum LDH, normal pH and glucose levels, and no detectable pathogenic microorganisms. During this stage, effective drainage of pleural effusion facilitates lung re-expansion.
Stage 2 (Purulent and Fibropurulent Phase)
With disease progression, the exudate transitions from serous to purulent. The pleural effusion increasingly contains pus cells and fibrin, with fibrin progressively depositing on the surfaces of the visceral and parietal pleura and forming a fibrinous layer. This can divide the pleural fluid into multiple small loculated pockets. Characteristics of the pleural fluid during this stage include a pH < 7.2, glucose concentration < 2.2 mmol/L, and LDH > 1,000 IU/L. At the early stage of this phase, the fibrinous membrane remains loosely adherent, soft, and easily removable.
Stage 3 (Chronic Organizing Phase)
With continued thickening of the fibrinous layer, scar tissue forms on the surfaces of both the visceral and parietal pleura. In the late stage, granulation tissue develops due to capillary and inflammatory cell proliferation, while fibrin deposition becomes organized and forms a dense, rigid fibrous plate which constitutes the walls of the empyema cavity. These fibrous plates may intrude into the lung tissue, limiting pulmonary expansion, impairing lung function, and creating an empyema cavity capable of sustaining chronic infection.
While the aforementioned pathological changes in empyema are divided into distinct stages, there are no precise time boundaries separating them, and clinical presentations may vary. Therefore, comprehensive assessment of the stages of empyema is critical for formulating appropriate treatment strategies.
To be continued