Etiology
The main causes include:
- Untreated acute empyema;
- Improper management of acute empyema, such as delayed drainage, premature removal of the drainage tube, use of excessively thin drainage tubes, or improper tube positioning leading to inadequate pus drainage;
- The presence of retained foreign bodies in the empyema cavity, making pleural cavity infections difficult to control;
- Associated complications, such as unaddressed bronchopleural or esophagopleural fistulas, or repeated infections from chronic infectious foci adjacent to the pleural cavity (e.g., subdiaphragmatic abscess, hepatic abscess, or rib osteomyelitis), resulting in the failure of cavity closure;
- Infections caused by specific pathogens, including Mycobacterium tuberculosis or fungal infections.
Pathology
Chronic empyema is characterized by fibrotic thickening of the visceral and parietal pleura, which forms a dense and tough-walled empyema cavity. These changes restrict lung expansion and prevent the reduction of the empyema cavity, making infection difficult to control. Thickening of the parietal pleura can also lead to narrowing of the intercostal spaces and thoracic collapse. Contraction of the cavity wall can cause mediastinal shift toward the affected side. These changes severely impair respiratory function, and some patients may develop clubbing of the fingers or toes.
Clinical Manifestations and Diagnosis
Patients often present with chronic systemic toxicity symptoms, including prolonged low-grade fever, loss of appetite, weight loss, anemia, and hypoproteinemia. Additional symptoms such as breathlessness, coughing, and purulent sputum may occur at times. Physical examination and chest imaging may reveal changes consistent with these findings. In patients who have previously undergone closed thoracic drainage, drainage tube scars or fistulas may be visible on the chest wall. The diagnosis of chronic empyema can be confirmed based on the patient’s history, clinical signs, and chest CT imaging.
Treatment
The treatment of chronic empyema aims to eliminate the causative factors and the empyema cavity through surgical methods, allowing the compressed lung to re-expand and restoring pulmonary ventilation. Common surgical approaches include:
Decortication
This procedure removes the fibrous layers of the parietal and visceral pleura surrounding the empyema cavity, enabling lung expansion, elimination of the empyema cavity, and improvement of pulmonary function and thoracic respiratory movement. It is one of the primary treatment methods for chronic empyema. Historically, open thoracotomy was utilized for decortication; however, video-assisted thoracoscopic surgery (VATS) is now commonly performed due to its minimally invasive nature, offering comparable efficacy in most cases. Nonetheless, this procedure is unsuitable for patients with long-standing disease or excessively thick fibrous layers. Additionally, it is contraindicated in patients with prolonged lung collapse, where pulmonary tissue has become fibrotic and unable to expand, or in those with extensive pulmonary diseases, such as tuberculous cavitation or bronchiectasis. In such cases, pleuropneumonectomy is recommended instead.
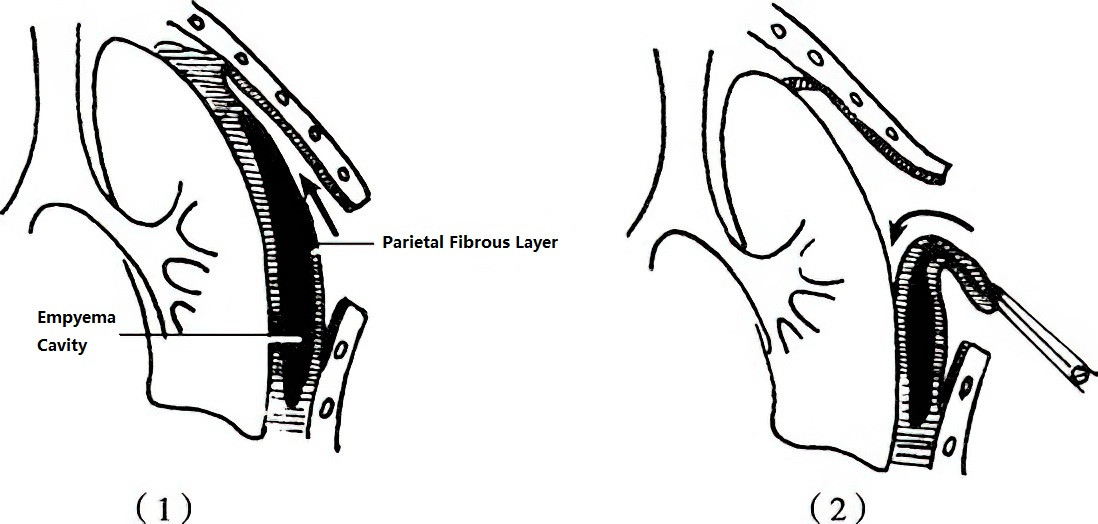
Figure 1 Decortication procedure (Illustration)
(1) Removal of the parietal pleural fibrous layer
(2) Removal of the visceral pleural fibrous layer
Thoracoplasty
The objective of this procedure is to eliminate the dead space between the two pleural layers by removing rigid structures in the thoracic wall, causing the chest wall to collapse inward. During surgery, portions of the ribs overlying the empyema cavity and the thickened fibrous layer of the parietal pleura are removed, while preserving intercostal neurovascular bundles, intercostal muscles, and rib periosteum. These preserved soft tissues can form pedicled flaps to fill the empyema cavity or close bronchopleural fistulas. For larger empyema cavities, pedicled muscle flaps such as the latissimus dorsi or serratus anterior, or pedicled omental grafts, may be used to fill the cavity. In patients with poor overall health who cannot tolerate an extensive one-time surgery, a staged approach from top to bottom may be adopted, with an interval of approximately three weeks between stages. Due to its significant invasiveness, thoracoplasty is rarely performed in modern practice.
Pleuropneumonectomy
For cases of chronic empyema associated with severe pulmonary disease—such as extensive bronchiectasis, tuberculous cavitation, fibrosis with dense consolidation, or unrepaired bronchopleural fistulas—complete removal of the affected lung and fibrous layers may be performed during the same surgery. This procedure is highly technically demanding, involves significant blood loss, and is associated with considerable surgical trauma. Indications for this procedure must be strictly evaluated.