Anterior uveitis includes three types: iritis, iridocyclitis, and anterior cyclitis. It is the most common type of uveitis, accounting for approximately 50% of all uveitis cases.
Based on etiology and disease course, anterior uveitis can be broadly categorized into three types:
- Acute anterior uveitis, commonly associated with HLA-B27 positivity, which may occur alongside ankylosing spondylitis, psoriatic arthritis, reactive arthritis, and inflammatory bowel disease.
- Chronic anterior uveitis, such as Fuchs uveitis syndrome and pediatric idiopathic uveitis.
- Conditions that can present with both acute and chronic inflammation, such as juvenile idiopathic arthritis, tuberculosis, or syphilis.
Clinical Presentation
Symptoms
Acute inflammation may manifest as eye pain, photophobia, tearing, and blurred vision. When significant fibrin exudation is present in the anterior chamber, or in cases of reactive macular edema or optic disc edema, vision may decrease noticeably. Chronic inflammation may present with mild or no symptoms but is associated with a higher risk of complications such as secondary cataracts or secondary glaucoma, which can lead to significant visual impairment.
Signs
Ciliary or Mixed Injection
Ciliary injection refers to congestion of the superficial scleral vessels around the limbus and is a common sign of acute anterior uveitis. Similar injection patterns may also be seen in conditions such as keratitis or acute angle-closure glaucoma, and careful differentiation is necessary.
Keratic Precipitates (KP)
Inflammatory cells or pigments that deposit on the posterior corneal surface are referred to as KP. The formation of KP requires concurrent corneal endothelial injury and the presence of inflammatory cells or pigments. Based on their appearance, KP can be categorized into three types:
- Fine granular KP: Typically found in non-granulomatous anterior uveitis, though it can also appear in certain stages of granulomatous uveitis.
- Medium-sized KP: Commonly seen in conditions such as Fuchs uveitis syndrome, glaucomatocyclitic crisis, and anterior uveitis associated with viral keratitis.
- Mutton-fat KP: Mainly composed of monocytes, macrophages, and epithelioid cells, these are characteristic of granulomatous uveitis.
KP distribution patterns include:
- Triangular distribution in the inferior corneal region, the most common pattern.
- Distribution within the central pupillary zone of the cornea, typical of Fuchs uveitis syndrome, glaucomatocyclitic crisis, and anterior uveitis secondary to viral keratitis.
- Diffuse distribution across the posterior corneal surface, often seen in Fuchs uveitis syndrome and anterior uveitis associated with viral keratitis.
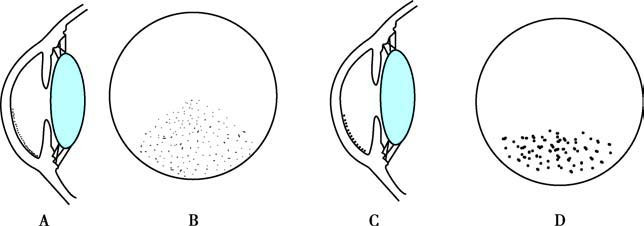
Figure 1 Schematic diagram of KP morphology and distribution patterns in uveitis patients
A and B depict medium-sized KP with a triangular distribution in the inferior corneal region.
C and D depict mutton-fat KP distributed in the inferior corneal region.
Anterior Chamber Flare
This presentation results from blood-aqueous barrier dysfunction, allowing proteins to enter the aqueous humor. It appears as a beam of white light in the anterior chamber when viewed under a slit-lamp microscope. Active anterior uveitis frequently leads to anterior chamber flare. However, even after inflammation subsides, the damaged blood-aqueous barrier may take time to recover, so anterior chamber flare may persist. Other conditions, such as acute angle-closure glaucoma or blunt trauma, can also disrupt the blood-aqueous barrier and produce anterior chamber flare. Thus, its presence does not necessarily indicate active inflammation and should not automatically warrant local glucocorticoid treatment.

Figure 2 Anterior chamber flare
A slit-lamp microscope reveals a white beam of light in the anterior chamber.
Anterior Chamber Cells
Pathological conditions may result in the presence of inflammatory cells, red blood cells, tumor cells, or pigment cells in the aqueous humor. In uveitis, these are predominantly inflammatory cells, seen as uniformly sized grayish-white dust-like particles under the slit-lamp microscope. These particles exhibit upward movement near the iris surface and downward movement near the corneal surface. Anterior chamber cells serve as a reliable indicator of anterior segment inflammation. When a large number of inflammatory cells accumulate in the inferior angle of the anterior chamber, a horizontal fluid level, known as hypopyon, may become visible. In severe inflammation, significant fibrinous exudation may occur, leading to a relatively coagulated state of the aqueous humor.
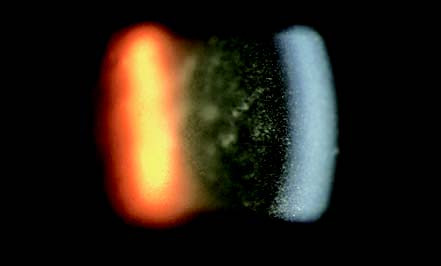
Figure 3 Anterior chamber cells
A slit-lamp microscope shows numerous uniformly sized dust-like particles in the anterior chamber.

Figure 4 Hypopyon
Approximately 2mm of white hypopyon can be observed at the bottom of the anterior chamber.
Iris Changes
Various alterations may occur in the iris during anterior uveitis. Fibrous exudation and proliferation between the iris and the anterior surface of the lens may lead to their adhesion, known as posterior synechia of the iris. Extensive posterior synechia can obstruct the flow of aqueous humor from the posterior chamber to the anterior chamber, resulting in increased pressure in the posterior chamber and forward bulging of the iris, a condition referred to as iris bombé. Adhesion of the iris to the posterior surface of the cornea is termed anterior synechia of the iris, and when this adhesion occurs at the angle of the anterior chamber, it is called goniosynechia.
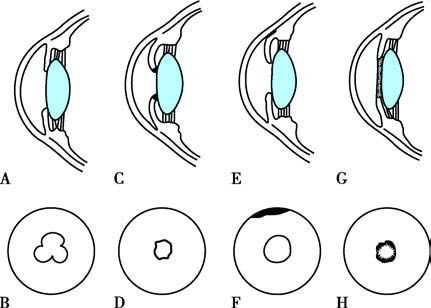
Figure 5 Schematic diagram of iris synechiae and pupil deformities
A. Focal posterior synechiae of the iris.
B. Cloverleaf-shaped pupil following dilation.
C. Circumferential posterior synechiae of the iris.
D. Seclusion of the pupil.
E. Anterior synechia of the iris occurring at the angle of the anterior chamber.
F. Formation of goniosynechiae.
G. Exudative membrane covering the entire pupillary area.
H. Formation of occlusion of the pupil.

Figure 6 Iris synechiae and seclusion of the pupil
A white membranous structure is observed in the pupillary zone, resulting in occlusion of the pupil. The arrow indicates a Busacca nodule.
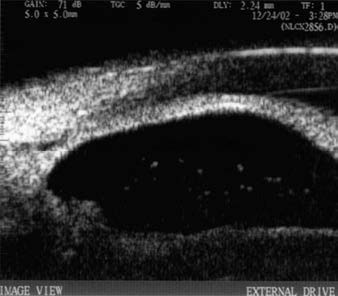
Figure 7 Anterior synechia of the iris (ultrasound biomicroscopy)
Ultrasound biomicroscopy shows adhesion between the iris and the posterior surface of the cornea at the angle of the anterior chamber, leading to the formation of goniosynechiae.
Inflammatory damage to the iris can lead to changes such as depigmentation, atrophy, and heterochromia. Inflammatory activity may also give rise to three types of nodules:
- Koeppe Nodules, which are nodules located near the pupillary margin. These can be observed in both non-granulomatous and granulomatous inflammation.
- Busacca Nodules, which are white or grayish translucent nodules found within the iris stroma, primarily present in granulomatous inflammation.
- Iris Granulomas, which are pink, opaque nodules occurring within the iris stroma, commonly seen in anterior uveitis associated with sarcoidosis.
Pupillary Changes
During inflammation, ciliary muscle spasm and sustained contraction of the pupillary sphincter muscle may lead to pupillary constriction. Partial posterior synechia of the iris may persist after being pulled apart, resulting in various irregular pupil shapes following dilation, such as cloverleaf, pear-shaped, or other irregular appearances. If the iris adheres 360° around its edge, the condition is referred to as seclusion of the pupil. When a fibrous membrane completely covers the pupillary area, this is known as occlusion of the pupil.
Lens Changes
Pigment deposition may occur on the anterior surface of the lens during anterior uveitis. After fresh posterior synechiae are separated, circular pigment deposits may remain on the anterior surface of the lens.
Vitreous and Posterior Segment Changes
In iridocyclitis and anterior cyclitis, inflammatory cells may be present in the anterior vitreous body. However, inflammation involving only the iris usually does not lead to inflammatory cells in the anterior vitreous. Generally, anterior uveitis does not result in vitreous opacities, but reactive cystoid macular edema or optic disc edema may occasionally occur.
Complications
Complicated Cataracts
Repeated episodes of inflammation or chronic inflammatory processes can alter the aqueous humor and affect lens metabolism, leading to cataract formation. This typically manifests as subcapsular posterior opacities in the lens. Additionally, long-term use of glucocorticoid eye drops during anterior uveitis can also contribute to posterior subcapsular lens opacities.
Secondary Glaucoma
Elevated intraocular pressure or secondary glaucoma may arise during anterior uveitis due to several factors:
- Obstruction of the trabecular meshwork by inflammatory cells, fibrinous exudates, and tissue debris.
- Peripheral anterior synechia of the iris or inflammation of the trabecular meshwork, leading to impaired aqueous outflow.
- Seclusion or occlusion of the pupil, both preventing aqueous humor from flowing from the posterior chamber to the anterior chamber.
Hypotony and Ocular Atrophy
Chronic or recurring inflammation may lead to detachment or atrophy of the ciliary body, reducing aqueous humor secretion and lowering intraocular pressure. Severe cases may result in ocular atrophy.
To be continued