Etiology and Pathology
Bacterial liver abscess occurs when systemic bacterial infections, particularly intra-abdominal infections, complicate in immunocompromised patients. Individuals with underlying conditions, especially diabetes, represent a high-risk population. Bacteria can invade the liver through the following pathways:
- Biliary Tract: Benign or malignant biliary obstruction that leads to suppurative cholangitis enables bacteria to ascend along the bile ducts, which is the primary cause of bacterial liver abscess.
- Portal Vein: Conditions such as gangrenous appendicitis or gastrointestinal diverticulitis may allow bacteria to breach the intestinal barrier and reach the liver via the portal vein.
- Hepatic Artery: Pyogenic lesions in other parts of the body, such as bacterial endocarditis or pyogenic osteomyelitis, can result in bacteremia, through which bacteria infiltrate the liver via the hepatic artery.
- Local Spread: Infections in organs or tissues adjacent to the liver can spread to the liver via lymphatic pathways or direct extension.
- Trauma: Open liver injuries allow direct bacterial invasion through the wound, leading to abscess formation.
Additionally, invasive procedures such as transarterial chemoembolization or ablation therapies can occasionally result in liver abscesses. In some cases, the exact cause of the liver abscess may remain unclear, which is then referred to as cryptogenic infection.
The common pathogens associated with bacterial liver abscess include Klebsiella pneumoniae, Escherichia coli, anaerobic streptococci, and Staphylococcus. Larger single abscesses may form in some cases, while multiple abscesses can range in size from a few millimeters to several centimeters, sometimes merging into one large abscess.
Clinical Manifestations
The classic symptoms of bacterial liver abscess include chills, high fever, liver pain, and hepatomegaly. Body temperatures often rise to 39–40°C, accompanied by nausea, vomiting, loss of appetite, and generalized weakness. Dull or distending pain in the liver area is often persistent and may radiate to the right shoulder. Pain in the lower right chest, liver tenderness upon percussion or palpation, and referred tenderness in the liver area are common. If the abscess is located superficially near the anterior inferior margin of the liver, right upper abdominal muscle tension and localized tenderness may occur. Large liver abscesses can cause bulging of the right hypochondrium and occasionally visible localized swelling with skin erythema and edema. Severe cases or those complicated by biliary obstruction may present with jaundice.
Liver abscesses in the right lobe may rupture through the liver capsule, leading to subphrenic abscesses or perforation into the right pleural cavity. Left lobe abscesses may rarely rupture into the pericardial cavity. Rupture into the abdominal cavity can result in acute peritonitis. In rare cases, abscesses may erode into blood vessels or bile ducts, causing profuse bleeding which may be expelled via the biliary tract, presenting clinically as upper gastrointestinal bleeding.
Laboratory findings may reveal elevated white blood cell counts and neutrophil percentages, along with increased liver enzymes, alkaline phosphatase, C-reactive protein (CRP), and erythrocyte sedimentation rate (ESR). Chronic cases may exhibit anemia and hypoalbuminemia. Ultrasound is the preferred diagnostic tool due to its ability to determine the location and size of the abscess, with a detection rate exceeding 96%. Computed tomography (CT) offers better visualization of multiple small abscesses, whereas magnetic resonance imaging (MRI) is particularly useful in suspected biliary disease. Chest and abdominal X-rays may show an elevated right hemidiaphragm, enlarged liver opacity, or localized liver bulge. Reactive pleuritis or pleural effusion may also occur on the right side.
Diagnosis
The diagnosis is established based on the patient’s history, clinical manifestations, laboratory findings, and ultrasound examination. If necessary, diagnostic aspiration with a needle at the area of maximal tenderness or under ultrasound guidance can confirm the diagnosis.
Differential Diagnosis
Bacterial liver abscess should primarily be differentiated from amebic liver abscess. Additionally, distinguishing it from subphrenic abscess, biliary infections, and liver malignancies, especially intrahepatic cholangiocarcinoma, is important.
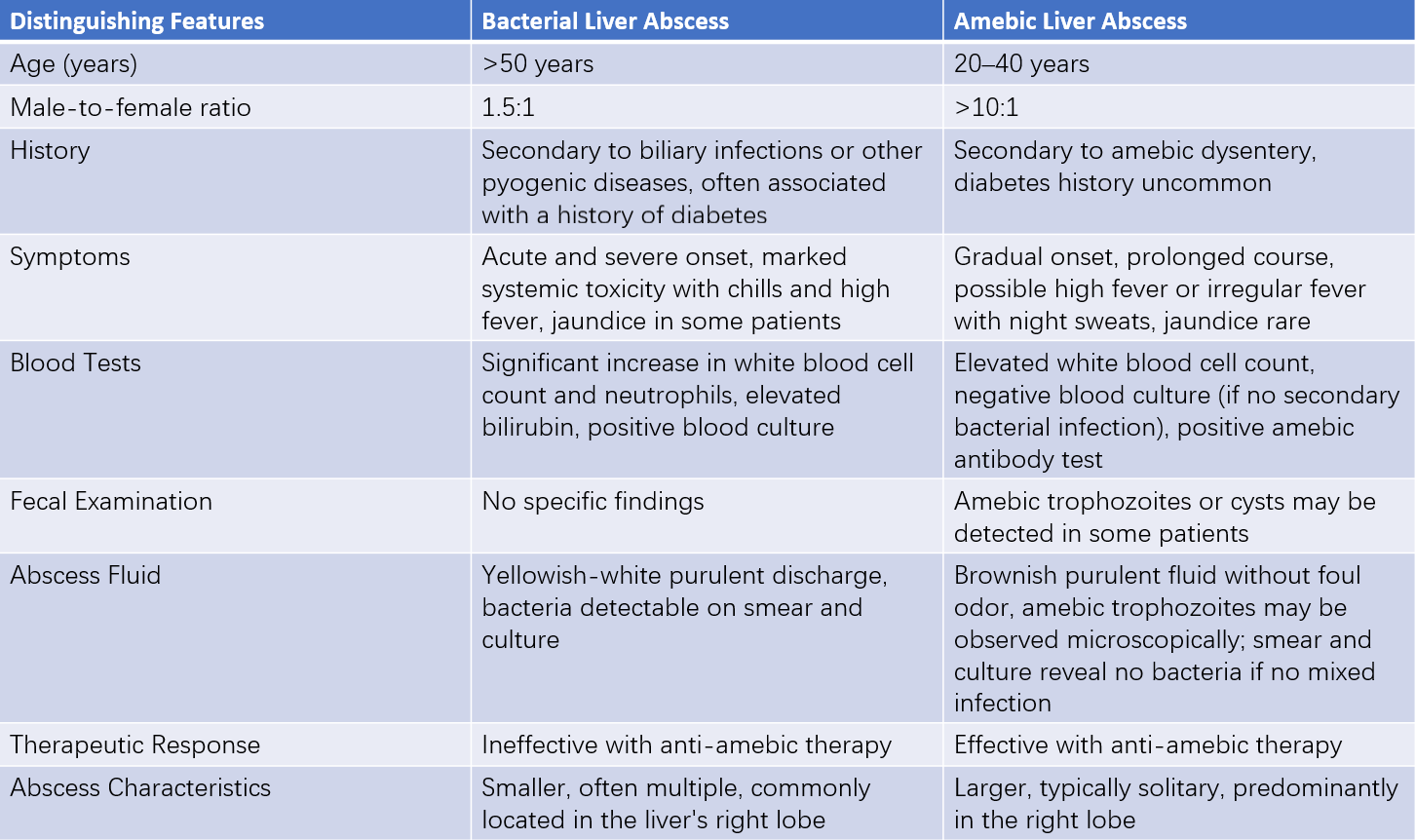
Table 1 Differential diagnosis of bacterial liver abscess and amebic liver abscess
Treatment
Early diagnosis and active treatment are critical for bacterial liver abscess management.
Systemic Supportive Therapy
Providing adequate nutritional support is essential. This may involve administering small, repeated doses of blood or plasma as needed to address anemia and correct hypoproteinemia. Immunity enhancement and correction of water and electrolyte imbalances are also important components of treatment.
Antibiotic Therapy
Initial treatment involves empirical broad-spectrum antibiotics when the causative pathogen has not been identified. Common regimens include third-generation cephalosporins combined with metronidazole, or ampicillin and aminoglycosides combined with metronidazole. Once bacterial culture results and antibiotic sensitivity testing are available, a switch to pathogen-specific antibiotics is recommended. Antibiotics should be administered in high doses and for an adequate duration to ensure effectiveness.
Percutaneous Hepatic Abscess Drainage
For single abscesses measuring 3–5 cm in diameter that have undergone liquefaction, percutaneous aspiration and catheter drainage can be performed under ultrasound or CT guidance. After catheter placement, isotonic saline may be used to slowly irrigate the abscess cavity, followed by the instillation of antibacterial agents starting from the second or subsequent day. Once the drainage catheter no longer yields purulent fluid, the patient’s general condition improves, the irrigation fluid becomes clear, and the abscess cavity shows significant shrinkage, removal of the catheter may be performed. Most cases of liver abscesses can be cured using a combination of antibiotics and percutaneous aspiration or catheter drainage.
Surgical Treatment
Surgical intervention is considered in cases with large or multiloculated abscesses, abscesses that have ruptured into the thoracic or abdominal cavity, biliary-origin liver abscesses, or chronic liver abscesses. The primary surgical approach involves incision and drainage, suitable for most patients. Laparoscopic drainage of liver abscesses is a preferred method, with open laparotomy now rarely used. During surgery, careful isolation of the abdominal cavity and surrounding organs with gauze is essential to prevent abscess fluid contamination. A multi-perforated rubber catheter is typically placed within the abscess cavity for drainage.
Special considerations during surgery include:
- If the abscess has ruptured into the pleural cavity, simultaneous drainage of the pleural cavity is necessary.
- In cases of biliary-origin liver abscess, biliary drainage is required.
- In blood-borne liver abscesses, aggressive management of the primary infection focus is necessary.
Chronic liver abscesses often require liver resection.