An anal fissure is a small ulcer that forms as a result of a full-thickness tear in the anal canal’s skin below the dentate line. It runs parallel to the anal canal's longitudinal axis and typically presents as spindle-shaped or oval, often leading to severe anal pain. Anal fissures are most common in young and middle-aged adults, with the vast majority occurring in the posterior midline of the anal canal. A smaller number affect the anterior midline, and very rarely, the fissures may be located laterally.
Etiology and Pathology
The exact cause of anal fissures remains unclear, though several potential contributing factors have been suggested:
Anatomical Factors
The posterior anal canal is more prone to injury because the superficial part of the external anal sphincter in this location forms a relatively inelastic and rigid band. Additionally, blood supply to this area may be poor. The angle between the anal canal and rectum increases pressure on the posterior wall of the anal canal during defecation, making it more susceptible to damage.
Traumatic Factors
Mechanical injury is the direct cause of anal fissure formation. Contributing factors include chronic constipation, hard stools, excessive straining during defecation, childbirth, and improper rectal examinations, all of which can damage the anal canal and lead to fissures.
Infectious Factors
Persistent inflammation is another important contributing factor in the development of anal fissures. Chronic inflammatory conditions such as perianal eczema, dermatitis, anal sinusitis, anal papillitis, or proctitis can result in fibrosis and reduced elasticity of anal canal skin, increasing its susceptibility to injury.
Chronic fissures are associated with certain pathological changes. At the upper end, edema and swelling of the anal papillae result in hypertrophied anal papillae. At the lower end, inflammation, edema, and impaired venous and lymphatic drainage cause the skin to protrude downward beyond the anal verge, forming a skin tag known as a sentinel pile. The fissure, sentinel pile, and hypertrophied anal papillae commonly coexist, forming the “anal fissure triad,” which is a hallmark clinical presentation.
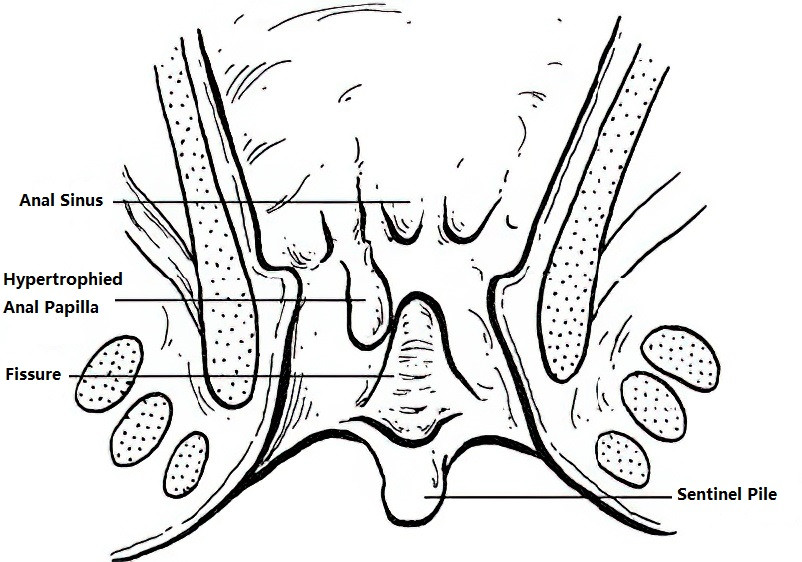
Figure 1 The “triad” of anal fissures
Clinical Manifestations
Pain
Pain is the primary symptom of anal fissures. During defecation, the exposed nerve endings in the fissure become irritated, leading to sharp, tearing, or knife-like pain. The pain temporarily subsides after defecation but may recur within a few minutes due to anal sphincter spasms. This pain may last for one to several hours before subsiding, only to reappear during the next bowel movement. This cyclic pattern of pain is a characteristic feature of anal fissures.
Bleeding
Post-defecation bleeding is common and may manifest as blood streaks on stool or bloody drops in the toilet bowl. The bleeding is usually bright red and occurs intermittently, caused by the fissure widening during defecation and tearing small blood vessels.
Constipation
Patients may avoid defecation due to fear of pain, leading to delayed bowel movements. Prolonged stool retention causes increased water absorption, resulting in harder stools that exacerbate pain upon defecation. This vicious cycle further delays healing and perpetuates the condition.
Diagnosis
The diagnosis of anal fissures is generally straightforward and relies on a detailed medical history combined with a thorough physical examination. A history of constipation and cyclic anal pain is typical. During rectal examination, acute fissures present as shallow, red, and elastic tears with smooth margins. Chronic fissures, on the other hand, are deeper with irregular and thickened edges, often showing fibrosis and grayish-white granulation tissue. In some cases, rectal examination may exacerbate the pain and require local anesthesia.
Differential Diagnosis
Anal fissures need to be differentiated from other conditions associated with perianal ulcers, including Crohn’s disease, ulcerative colitis, intestinal tuberculosis, anal canal carcinoma, chancroid, syphilis, and anal chapping.
Treatment
The primary treatment objectives are symptom relief, alleviation of sphincter spasms, breaking the vicious cycle of pain and constipation, and promoting local healing.
Acute or newly developed anal fissures can be treated with sitz baths and stool softeners.
Chronic anal fissures may require a combination of sitz baths, stool softeners, and anal dilation.
For fissures that fail to respond to conservative management or present with severe symptoms, surgical intervention may be necessary.
Non-Surgical Treatment
Dietary Adjustment
A diet rich in vegetables and fruits with increased intake of dietary fiber is recommended.
Stool Softening
Oral administration of laxatives or liquid paraffin helps maintain smooth bowel movements.
Warm Sitz Baths
Using warm water for sitz baths after defecation helps alleviate pain.
Anal Dilation
Manual or instrument-based dilation of the anal canal for 5 minutes is used as a method to treat anal fissures.
Surgical Treatment
Fissurectomy
This involves the excision of all hypertrophic and hardened fissure tissue, sentinel piles, hypertrophied anal papillae, inflamed crypts, and unhealthy deeper tissues until the anal sphincter is adequately exposed. The subcutaneous portion of the external anal sphincter or part of the internal anal sphincter may also be incised, and the wound is left open for drainage.
Internal Sphincterotomy
The internal anal sphincter, which is a ring-like involuntary muscle, is primarily responsible for pain caused by spasms. A small incision is created 1.0–1.5 cm from the anal verge at the posterior side to access and partially cut through the internal sphincter. The anal canal is dilated up to four fingers. After achieving hemostasis, the wound is left open. Hypertrophied anal papillae and sentinel piles may be removed simultaneously. This method demonstrates a high cure rate.
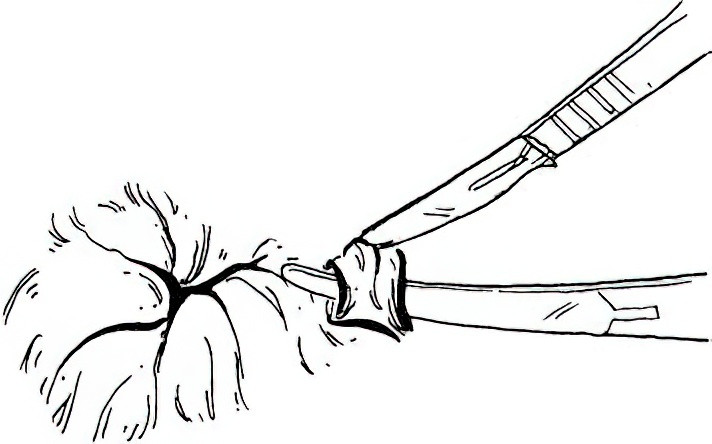
Figure 2 Internal sphincterotomy for anal fissures
Seton Procedure
This method is applicable for fissures accompanied by subcutaneous fistulas, nodular induration of the anal verge, or anal stenosis.