Ulcerative colitis (UC) is a diffuse inflammatory disease that occurs in the colon and rectum. It typically begins in the rectum and progresses proximally, although in rare cases, the terminal ileum may also be affected, a condition known as backwash ileitis. The lesions are usually confined to the mucosal and submucosal layers of the bowel wall, with minimal thickening. The affected mucosa often exhibits extensive edema, hyperemia, erosion, and ulceration. Clinically, bloody diarrhea is the most common early symptom, typically presenting as stools mixed with pus and blood. Abdominal pain tends to be mild to moderate, with cramping characteristics.
Indications for Surgical Treatment
The indications for surgical treatment of UC include toxic megacolon, perforation, massive hemorrhage, intolerable extraintestinal manifestations, and malignancy. Furthermore, as total proctocolectomy is a curative approach, surgery may also be considered in patients with persistent symptoms unresponsive to medical therapy.
Surgical Procedures
Surgical management primarily consists of three types of procedures:
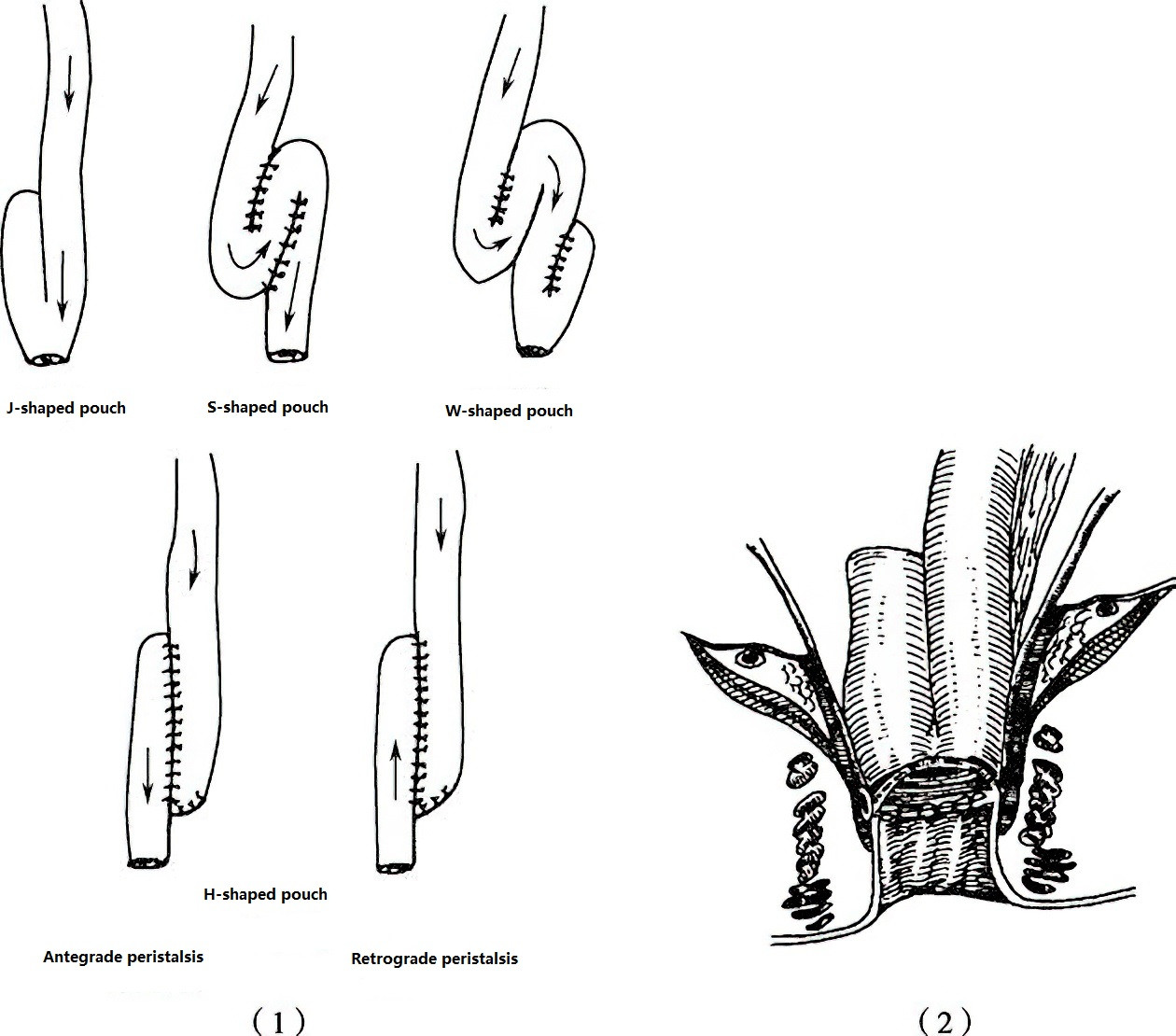
Figure 1 Ileal pouch-anal anastomosis
(1) Various types of ileal pouches (2) J-pouch anal anastomosis
Total Proctocolectomy with Ileostomy
This procedure has been in use since the 1930s. It involves the complete removal of all affected regions of the colon and rectum, eliminating the risk of disease recurrence and cancer development. However, the permanent ileostomy required in this approach may impact the patient's quality of life.
Colectomy with Ileorectal Anastomosis
Introduced in the early 1960s, this procedure was developed to preserve rectal and anal sphincter function, thereby avoiding a permanent ileostomy. However, as it does not remove all disease-prone areas, there remains a risk of recurrence and malignancy. For this reason, it has fallen out of favor over time.
Total Proctocolectomy with Ileal Pouch-Anal Anastomosis (IPAA)
This surgical technique has become the standard procedure for treating most cases of UC. Its advantages include the removal of all potentially diseased mucosa while preserving parasympathetic nerves to the bladder and reproductive organs, avoiding the need for a permanent ileostomy, and retaining anal sphincter function. Variations of the ileal pouch include J-shaped, S-shaped, W-shaped, and H-shaped configurations, with the J-pouch being the most commonly used.