Duodenal obstruction syndrome refers to luminal obstruction of the horizontal portion of the duodenum caused by compression from the superior mesenteric artery, also known as superior mesenteric artery syndrome.
Etiology and Pathology
The horizontal portion of the duodenum crosses from right to left across the spine and abdominal aorta at the level of the third lumbar vertebra. The superior mesenteric artery arises from the abdominal aorta at the lower edge of the pancreatic neck and passes from above to below, crossing the anterior surface of the horizontal part of the duodenum. If the angle between the superior mesenteric artery and abdominal aorta is reduced, the superior mesenteric artery compresses the horizontal portion of the duodenum against the spine or abdominal aorta, resulting in narrowing or obstruction of the duodenal lumen.
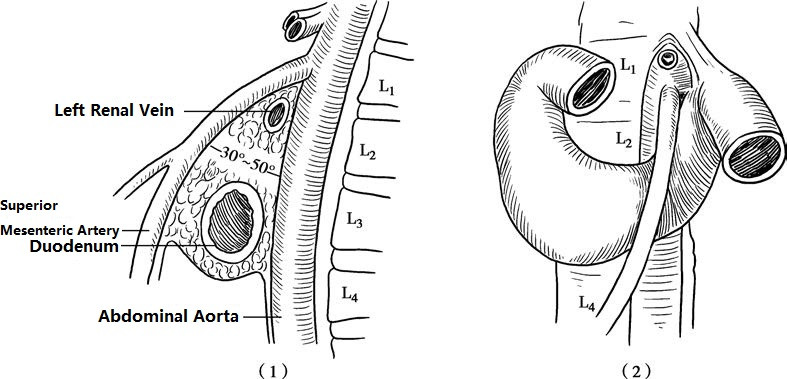
Figure 1 Duodenal obstruction syndrome
(1) Lateral View (2) Frontal View
The main causes of duodenal obstruction syndrome include a low origin of the superior mesenteric artery, a short duodenal suspensory ligament causing traction, intra-abdominal adhesions, visceral ptosis pulling on the mesentery, and conditions like annular pancreas. The average age of onset is approximately 30 years and is more common in underweight individuals with a lean and tall body type, or in those with a hypermetabolic state, such as patients with extensive burns or undergoing major surgeries.
Clinical Manifestations
Duodenal obstruction syndrome often presents as intermittent and recurrent episodes of duodenal obstruction. Vomiting is the predominant symptom, typically occurring 2–3 hours after meals or at night. The vomitus contains bile and gastric contents and may be accompanied by upper abdominal fullness, discomfort, or pain. Symptoms may alleviate with changes in body position, such as adopting a left lateral, prone, or knee-to-chest position, which is characteristic of the syndrome.
Physical examination may reveal a distended upper abdomen, visible gastric outline, and peristaltic waves, but there is usually no significant abdominal tenderness. Bowel sounds are normal, and gastric decompression may produce a large output of gastric fluid. In the remission phase, nonspecific gastrointestinal symptoms such as loss of appetite or postprandial fullness may be present. Patients with chronic and recurrent episodes may develop weight loss, malnutrition, anemia, and water-electrolyte imbalances.
Diagnosis
The possibility of this condition should be considered in patients with recurrent vomiting of bile and gastric contents, especially when symptoms improve with changes in body position. Barium study with X-ray is the preferred diagnostic method, with characteristic findings including:
- Dilatation of the proximal duodenum and stomach, with significant retrograde peristalsis in the duodenum;
- Interruption of the barium column at the midline of the horizontal part of the duodenum, showing a slanted indentation resembling a "pencil sign" due to vascular compression, with impaired passage of contrast;
- Delayed gastric emptying, with barium persisting in the duodenum for 2–4 hours;
- Improved passage of barium through the horizontal part of the duodenum in the lateral or prone position.
Ultrasound can measure the angle between the superior mesenteric artery and the abdominal aorta, which normally ranges from 30° to 50°. In patients with duodenal obstruction syndrome, the angle is less than 13°. The anteroposterior diameter of the compressed horizontal portion of the duodenum is less than 1.0 cm, while the anteroposterior diameter of the proximal descending portion exceeds 3.0 cm. Body position changes can also alter these measurements. CT combined with angiography can provide detailed visualization of the relationship between the superior mesenteric artery and the duodenum, as well as the obstruction at the corresponding level.
Treatment
Non-surgical treatment is generally prioritized. Management during episodes includes rest, fasting, gastric decompression, maintenance of fluid and electrolyte balance, and nutritional support. During remission, patients are encouraged to consume small, frequent meals consisting of easily digestible foods. Adopting a lateral or prone position after meals may prevent recurrent episodes.
Surgical treatment is indicated when non-surgical measures are ineffective. The most commonly performed procedure is duodenojejunostomy, which creates a side-to-side anastomosis between the proximal horizontal duodenum and the first part of the jejunum, or a Roux-en-Y anastomosis. If the compression is caused by a short suspensory ligament of the duodenum, division and release of the ligament may be performed.