Apart from perforation repair and bleeding ligation procedures, the main surgical approach is open or laparoscopic partial gastrectomy. Indications for surgery include failure of conservative treatment for gastric and duodenal ulcers or complications such as perforation, bleeding, pyloric obstruction, or malignancy. Partial gastrectomy involves the resection of gastric tissue and the reconstruction of gastrointestinal continuity.
Extent of Gastric Resection
The resection typically involves removing two-thirds to three-fourths of the distal stomach, including the pylorus and part of the duodenal bulb. This resection eliminates a significant portion of the distal stomach, which contains a high concentration of parietal and chief cells, thereby reducing gastric acid and pepsin secretion. It also removes the antrum, which contains G cells, lowering gastrin secretion and reducing its stimulatory effect on gastric acid production, as well as excising ulcer-prone areas. The anatomical landmarks for the resection line are defined by the first branch of the left gastric artery along the lesser curvature to the last branch of the left gastroepiploic artery along the greater curvature, enabling the removal of approximately 60% of the stomach.
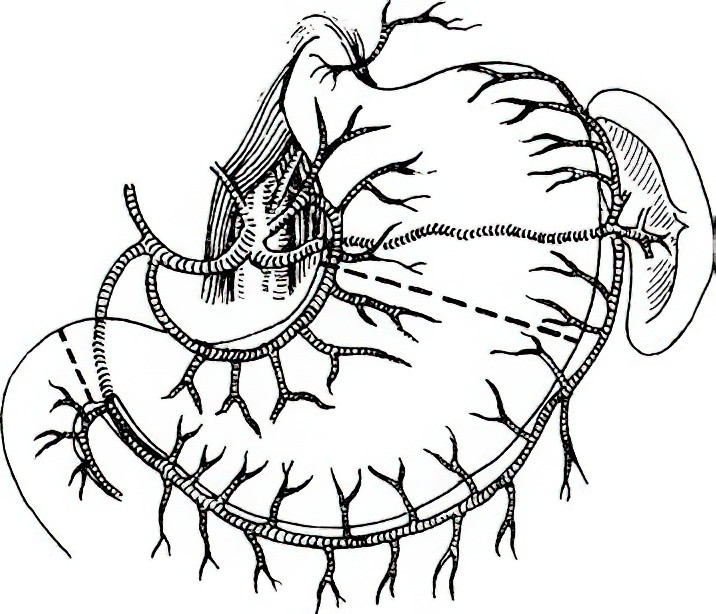
Figure 1 Extent of gastric resection
Reconstruction of Gastrointestinal Continuity
Reconstruction methods, chosen based on intraoperative conditions, include Billroth I, Billroth II, or Roux-en-Y gastrojejunostomy.
Billroth I Reconstruction
The remaining stomach is anastomosed to the duodenum, preserving the physiological continuity of the gastrointestinal tract. It is essential for the anastomosis to be tension-free. If tension is present, alternative reconstruction methods are used.
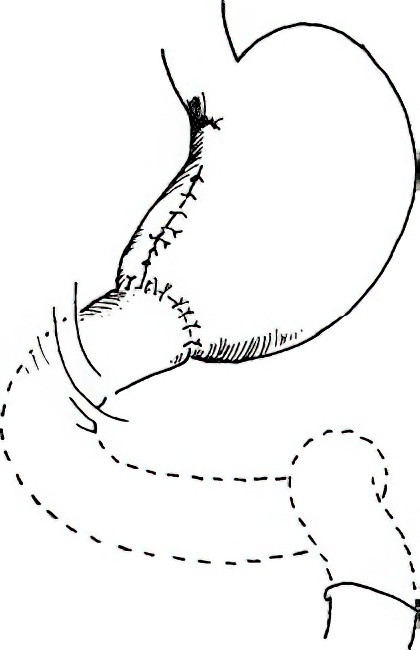
Figure 2 Billroth I reconstruction following partial gastrectomy
Billroth II Reconstruction
After closure of the duodenal stump, the gastric remnant is anastomosed to a jejunal loop. Based on the method of anastomosis, this can be categorized into antecolic and retrocolic approaches:
- Antecolic Approach: The jejunal loop is brought anterior to the transverse colon and anastomosed to the gastric stump.
- Retrocolic Approach: The transverse mesocolon is perforated, and the jejunal loop is brought posterior to the transverse colon and anastomosed to the gastric stump.
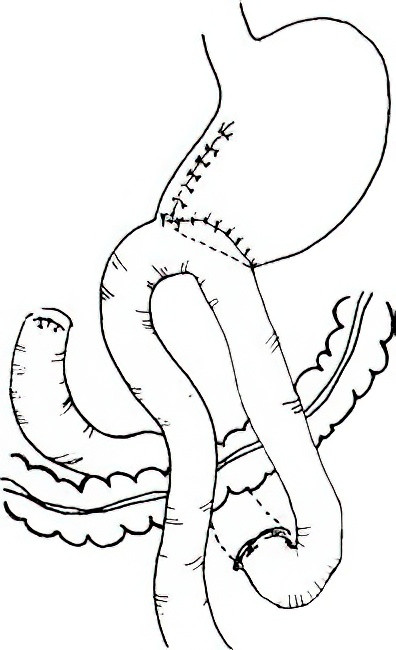
Figure 3 Billroth II reconstruction following partial gastrectomy
The anastomotic diameter is typically 3 to 4 cm. A diameter that is too large increases the risk of dumping syndrome, while one that is too small may impair gastric emptying. The length of the jejunal loop between the ligament of Treitz and the anastomosis is generally 8–10 cm in the antecolic approach and 6–8 cm in the retrocolic approach. During gastrojejunostomy, the proximal jejunal portion is positioned on either the lesser or greater curvature of the stomach based on intraoperative conditions and surgeon preference. The proximal jejunal portion should be higher than the distal part to facilitate gastric emptying. Specific techniques include:
- Hoffmeister Method: Partial gastric stump anastomosis with the jejunum in a retrocolic approach, with the afferent loop aligned with the lesser curvature.
- Moynihan Method: Complete gastric stump anastomosis with the jejunum in an antecolic approach, with the afferent loop aligned with the greater curvature.
Roux-en-Y Gastrojejunostomy
After closure of the duodenal stump, the gastric remnant is anastomosed to a jejunal limb. The jejunum is transected 10–15 cm distal to the ligament of Treitz. The distal stump is anastomosed to the stomach, while the proximal stump is side-to-side anastomosed to the jejunum approximately 45–60 cm distal to the gastrojejunostomy site. This procedure reduces reflux of bile and pancreatic secretions into the gastric remnant, thereby preventing reflux gastritis.
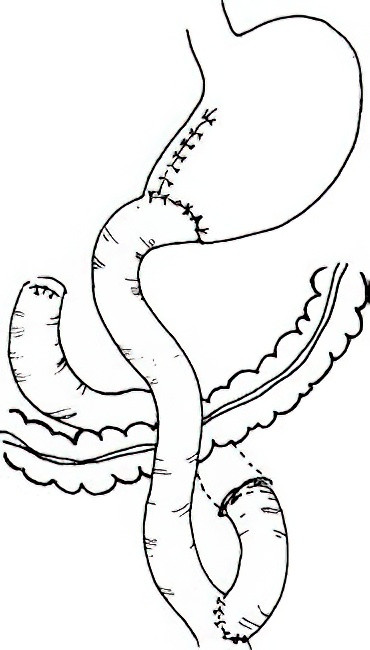
Figure 4 Roux-en-Y gastrojejunostomy after partial gastrectomy
Assessment of Surgical Outcomes
The outcomes of surgery can be graded using the Visick classification system:
- Grade I: Excellent recovery postoperatively, with no significant symptoms.
- Grade II: Mild gastrointestinal symptoms such as occasional abdominal discomfort or diarrhea, which can be managed with dietary adjustments and do not impact daily life.
- Grade III: Symptoms such as mild to moderate dumping syndrome or reflux gastritis that require pharmacological treatment but allow the patient to continue working and maintain normal living activities.
- Grade IV: Serious complications or ulcer recurrence that prevent normal work and daily life.
The recurrence rate of ulcers following partial gastrectomy is 2%–5%.