Gastrointestinal stromal tumors (GIST) are the most common mesenchymal tumors of the digestive tract, accounting for 1% to 3% of all digestive tract tumors. Among these, 60% to 70% occur in the stomach, 20% to 30% in the small intestine, and 10% in the colon and rectum. They can also occur in the esophagus, omentum, and mesentery. Previously, due to the lack of diagnostic markers, these tumors were often confused with smooth muscle (sarcoma) tumors or neurogenic tumors, which are also of mesenchymal origin in the gastrointestinal tract. Research has shown that these tumors originate from undifferentiated interstitial cells of the gastrointestinal tract. A key molecular biological feature is a mutation in the C-kit gene, leading to continuous activation of tyrosine kinase receptors, which stimulates persistent tumor cell proliferation. The C-kit gene encodes the KIT protein (CD117), serving as an important diagnostic marker.
Pathology
GISTs exhibit an expansive growth pattern and may infiltrate the submucosa or serosa, forming spherical or lobulated masses. The tumor can be solitary or multiple, with diameters ranging from 1 cm to over 20 cm. The texture is firm, with well-defined borders, and the surface appears nodular. Larger tumors may exhibit internal hemorrhage, necrosis, and cystic degeneration. Ulcers may form on the mucosal surface, leading to gastrointestinal bleeding.
Clinical Manifestations
Symptoms depend on the tumor's location, size, and growth pattern. Small tumors may present with nonspecific symptoms, such as epigastric discomfort or gastrointestinal symptoms similar to peptic ulcers. Larger tumors may be palpable as abdominal masses. Tumors infiltrating the gastrointestinal lumen often present with gastrointestinal bleeding. Small intestinal GISTs frequently cause intestinal obstruction and bleeding. GISTs located in the duodenum may compress the common bile duct, resulting in obstructive jaundice.
Diagnosis
Gastroscopy may reveal submucosal masses with central ulcers at the apex. GISTs are primarily located within the muscularis propria, and since the mucosa is often intact, biopsy specimens from the mucosa have a low diagnostic yield. Endoscopic ultrasound (EUS) can help determine the tumor's origin. CT and MRI scans are useful in identifying extraluminal nodular masses and assessing the presence of tumor metastasis. Histological examination of tissue samples often reveals spindle-shaped cells, and immunohistochemical testing frequently shows overexpression of CD117 and/or DOG-1, aiding in the definitive pathological diagnosis. GISTs are considered tumors with malignant potential, and tumor risk is associated with factors such as location, size, mitotic index, depth of invasion, and the presence of metastasis.
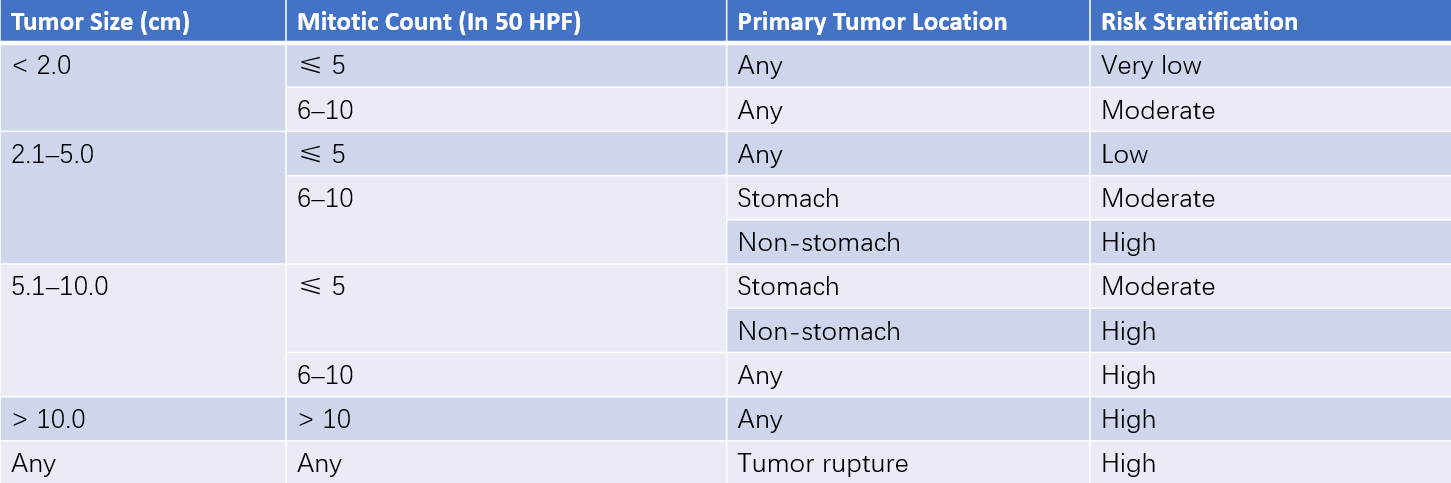
Table 1 Risk stratification of gastrointestinal stromal tumors (GIST)
Treatment
Surgical excision is the treatment of choice, with the goal of achieving complete and intact resection. Tumor rupture during surgery should be avoided. Lymph node and distant metastases are rare in GIST, so routine lymphadenectomy is not typically necessary. Patients with complete tumor removal have significantly better survival rates than those with incomplete resection. Imatinib mesylate, a tyrosine kinase inhibitor, targets C-kit activity and is effective in approximately 50% of cases of unresectable or recurrent and metastatic GIST. For intermediate- to high-risk GISTs, postoperative imatinib therapy can reduce recurrence and improve prognosis. It can also be used as neoadjuvant therapy to improve the resectability of tumors before surgery.