Primary lower extremity deep vein valve insufficiency refers to the inability of the deep venous valves to close tightly, leading to blood reflux without any congenital or secondary causes.
Etiology and Pathophysiology
The exact cause remains unclear, but several factors are associated with the condition:
- Structural weakness of the valves, where, under sustained retrograde blood flow and the gravitational pressure of the blood column, the free edges of the valves become lax and fail to close tightly, allowing venous reflux.
- Persistent volume overload returning to the heart causes dilation of the venous lumen, rendering the valves relatively shorter and insufficient for complete closure.
- Developmental abnormalities or absence of the deep venous valves result in the loss of normal closure function.
- Weakness in the calf muscle pump reduces its efficiency, leading to blood pooling in the veins, venous hypertension, and valve insufficiency.
The first pair of valves in the femoral vein often experience the brunt of retrograde blood flow from the proximal deep veins, making them the earliest to become incompetent. The opening of the deep femoral vein is relatively angled outward, thus being less affected by gravitational blood pressure, and valve dysfunction in this segment tends to occur later.
Clinical Manifestations and Diagnosis
Apart from superficial varicose veins, the severity of clinical manifestations can classify the condition as follows:
- Mild: Symptoms include a sense of heaviness or discomfort in the lower limbs after prolonged standing and mild ankle edema.
- Moderate: Symptoms include mild skin hyperpigmentation, subcutaneous fibrosis, and single small ulcers. There is a distinct feeling of heaviness in the lower limb, and moderate ankle swelling is present.
- Severe: Symptoms include leg swelling or a sense of heaviness after minimal activity. Marked swelling extends to the lower leg, accompanied by widespread hyperpigmentation, eczema, or multiple recurrent ulcers (either healed or active).
Since superficial varicose veins are a common symptom in various conditions, functional testing of the deep venous valves is necessary for a definitive diagnosis.
Venography
Antegrade venography of the lower extremities reveals the following characteristics: the deep veins are fully patent but exhibit significant dilation; the valve contours appear blurred or absent, losing the normal beaded (segmented) morphology and instead forming a cylindrical shape. During the Valsalva maneuver, reflux of contrast-enhanced blood from the proximal to the distal side of the valve can be observed. On retrograde venography, the contrast medium shows distal reflux.
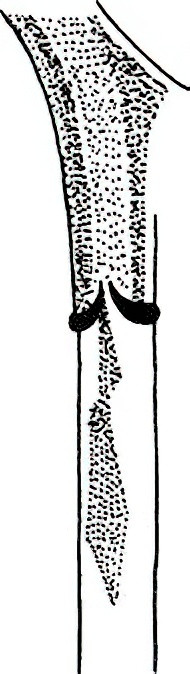
Figure 1 Retrograde venography of the lower limb
During deep vein valve insufficiency, contrast medium refluxes from the proximal to the distal side of the valve.
Lower Limb Dynamic Venous Pressure Measurement
This is often used as a screening test, it indirectly assesses valve function. In healthy individuals, the dorsal foot superficial vein pressure averages 10–30 mmHg following activity in a standing position. In primary varicose veins, the pressure rises to 25–40 mmHg, and in deep vein valve insufficiency, it can reach 55–85 mmHg.
Ultrasound Examination
This imaging modality allows observation of valvular closure activity and the presence of retrograde blood flow. Differentiation between primary deep vein valve insufficiency and post-thrombotic syndrome (PTS) is essential, as their clinical presentations are similar but their management differs. In PTS, there is often a history of deep vein thrombosis. The superficial varicose veins are extensive and may involve the lower abdominal wall. Venography shows partial or complete recanalization of the deep veins, irregular lumens, open collateral vessels, and the disappearance of valve shadows. In primary deep venous valve insufficiency, there is no history of deep vein thrombosis. Superficial varicose veins are confined to the lower limb, and venography reveals patent but dilated deep veins with a cylindrical shape and blurred valve shadows.
Treatment
Due to the unsatisfactory mid- and long-term outcomes of deep vein valve reconstruction surgeries, these procedures are now rarely performed. For patients with deep vein valve insufficiency associated with superficial varicose veins, current recommendations favor performing high ligation of the great saphenous vein, stripping of varicose tributaries, and ligation of incompetent perforating veins.