Peripheral arterial aneurysms refer to localized, abnormal dilations occurring in arterial regions outside the aorta. These may involve arteries of the extremities, carotid arteries, or subclavian arteries, with femoral and popliteal aneurysms being the most common, accounting for approximately 90% of peripheral arterial aneurysms. They are classified into three types:
- True arterial aneurysms
- False arterial aneurysms
- Dissecting aneurysms
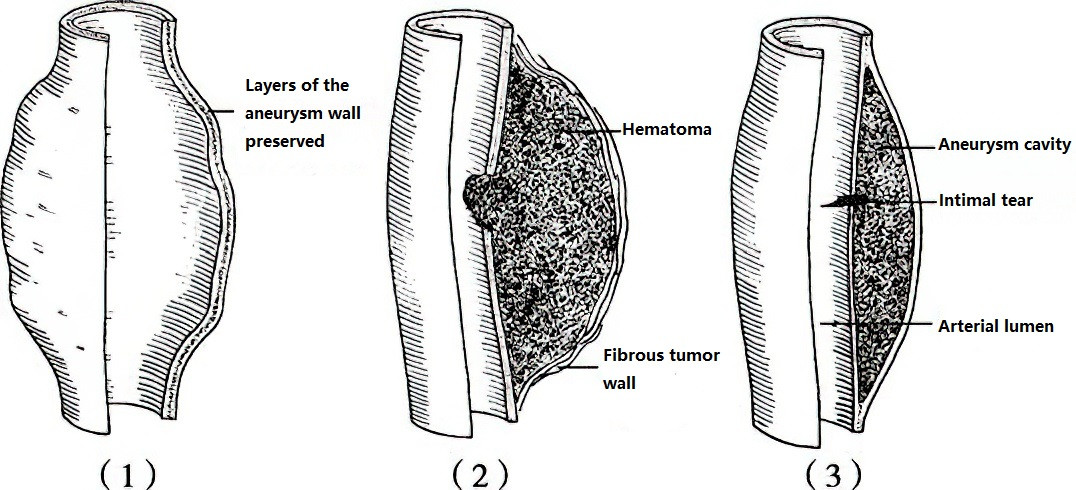
Figure 1 Classification of peripheral arterial aneurysms
1, True Aneurysm
2, False Aneurysm
3, Dissecting Aneurysm
Etiology
Peripheral arterial aneurysms have complex causes. Atherosclerosis is the most common reason for true aneurysms, while false aneurysms are often caused by trauma, infections, or inflammation.
Atherosclerosis
This frequently occurs in individuals aged 50 or above and is often accompanied by hypertension, coronary artery disease, or arteriosclerosis in other regions. It can manifest as multiple aneurysms.
Trauma
Sharp injuries, such as stab wounds, and blunt injuries, such as crushes or damage from bone fractures, are common causes. Chronic friction or compression of the axillary artery caused by long-term crutch usage and repeated arterial punctures among intravenous drug users are additional contributors. Iatrogenic injuries, including arterial punctures, catheterization, or arterial anastomoses, can also be causative factors.
Infections
Bacteria from conditions such as tuberculosis, infective endocarditis, or septicemia may invade the arterial wall through the bloodstream, forming small abscesses or micro-infections. These can lead to wall rupture and the development of infective arterial aneurysms. In some cases, syphilitic spirochetes affect the arterial wall, causing arterial inflammation and degeneration of collagen and elastic fibers in the tunica media, resulting in saccular or fusiform aneurysms.
Inflammatory arterial diseases: Nonbacterial inflammatory conditions, such as Takayasu arteritis, Kawasaki disease, or Behçet’s syndrome, frequently involve the arterial systems of young individuals, leading to aneurysm formation. Aneurysms arising in this context often show multiple occurrences and carry a high risk of rupture during active periods of inflammation.
Congenital Defects in the Arterial Media
Conditions such as Marfan syndrome and Ehlers-Danlos syndrome, typically seen in younger individuals, may predispose to aneurysm development.
Clinical Manifestations
Pulsatile Mass and Murmur
The most typical clinical presentation involves a smooth-surfaced mass that exhibits expansile pulsations, which are synchronous with the heartbeat. Thrills and systolic murmurs may also be detected.
Compression Symptoms
Symptoms arise from the aneurysm pressing on surrounding nerves, veins, or nearby organs. For instance, a carotid aneurysm compressing the recurrent laryngeal nerve may lead to unilateral vocal cord paralysis and hoarseness. Compression of sympathetic nerves in the neck may lead to Horner syndrome, while tracheal compression can cause respiratory difficulties, and esophageal compression may result in dysphagia.
Ischemia in Distal Limbs or Organs
Thrombus or atheromatous plaque fragments within the aneurysm cavity may embolize, causing distal arterial occlusion. Secondary thrombus formation can result in acute ischemia of downstream tissues.
Aneurysm Rupture
Continuous expansion of the aneurysm under pressure may eventually lead to sudden rupture and hemorrhage, posing a life-threatening emergency.
Other Symptoms
Rapid enlargement or impending rupture of the aneurysm may cause localized severe pain. Infective arterial aneurysms may present with local pain, redness, and swelling of surrounding tissues, as well as systemic symptoms such as fever or malaise.
Diagnosis and Differential Diagnosis
Diagnosis is usually based on clinical symptoms and physical examination. Small aneurysms or cases involving obese patients may be difficult to detect, increasing the likelihood of missed diagnoses. When aneurysms are accompanied by surrounding tissue inflammation or intraluminal thrombus, pulsation may not be prominent, leading to misdiagnoses as abscesses or benign tumors, which could result in unnecessary procedures such as biopsies or drainage. Popliteal aneurysms with thrombus formation should be differentiated from Baker's cysts.
Imaging studies, including Doppler ultrasound, DSA (digital subtraction angiography), CTA (computed tomography angiography), or MRA (magnetic resonance angiography), aid in confirming the diagnosis.
Treatment
Once diagnosed, peripheral arterial aneurysms require timely intervention. There are three main treatment approaches:
Surgical Treatment
This approach involves resecting the aneurysm and performing arterial reconstruction. Arterial reconstruction techniques include arterial patch repair, end-to-end anastomosis, or arterial grafting using artificial materials or autologous veins in cases with significant defects. For infected aneurysms with surrounding tissue involvement, removal of infected thrombus and thorough debridement are necessary, followed by vascular reconstruction, typically bypassing the infected area.
Endovascular Aneurysm Repair
This minimally invasive approach involves placing a covered stent within the affected arterial segment to exclude the aneurysm and simultaneously restore arterial continuity. While less invasive, this method can be more expensive than open surgery and is reserved for carefully selected cases.
Combination of Open and Endovascular Repair
This hybrid approach involves a smaller open surgery to reconstruct critical arterial branches affected by the aneurysm, followed by the use of a covered stent to isolate the aneurysm. It is suitable for deeply located aneurysms, cases where open surgery carries significant trauma, or patients unable to tolerate open surgical interventions. This method minimizes surgical trauma and reduces risks associated with the procedure.