Coronary atherosclerotic heart disease (coronary artery disease, CAD) is the most common cause of death due to heart disease in adults. This condition predominantly affects middle-aged and elderly individuals, with a significantly higher incidence in men than in women. The primary pathological changes include lipid deposits in the coronary artery intima, localized proliferation of connective tissue, fibrosis, or calcification, leading to the formation of atherosclerotic plaques. These changes result in thickened arterial walls, narrowed lumen, or complete occlusion.
Pathophysiology
In a healthy individual, the coronary blood flow at rest is approximately 250 ml per minute, accounting for 5% of cardiac output. Myocardial oxygen uptake is relatively stable, with approximately 150 ml of oxygen extracted from every 1,000 ml of coronary blood flow. During physical activity or emotional stress, increases in heart rate, contractility, and ventricular wall tension elevate myocardial oxygen demand. To meet this demand, coronary blood flow increases accordingly, compensating for the decreased arterial oxygen partial pressure. When coronary artery lumen narrowing prevents an increase in blood supply, myocardial ischemia symptoms manifest clinically as oxygen demand surpasses supply. Prolonged and severe myocardial ischemia may result in myocardial cell necrosis.
Clinical Manifestations
Patients with mild coronary lesions may remain asymptomatic regarding myocardial ischemia. Severe coronary lesions may reduce blood flow to a level sufficient only for resting myocardial oxygen needs. During physical exertion, emotional stress, or other conditions that increase myocardial oxygen demand, inadequate supply can exacerbate myocardial ischemia, resulting in angina pectoris. Symptoms typically include chest tightness, a compressive sensation behind the sternum, or episodic chest pain, which may radiate to the left shoulder, arm, elbow, or fingertips. Symptoms generally resolve with rest or the administration of vasodilators.
Prolonged coronary artery spasm or acute occlusion, coupled with thrombus formation, can lead to severe and persistent ischemia in a segment of the myocardium, causing localized myocardial infarction. Myocardial infarction is often characterized by severe and prolonged chest pain, which is typically unresponsive to rest or sublingual nitroglycerin. Additional symptoms may include nausea, vomiting, profuse sweating, arrhythmias, cardiogenic shock, heart failure, or ventricular wall rupture. Extensive myocardial necrosis due to prolonged ischemia may result in fibrous scarring and the formation of a ventricular aneurysm. If the infarction involves the papillary muscles, mitral regurgitation may occur. Involvement of the interventricular septum may result in septal perforation, leading to a ventricular septal defect. Chronic myocardial ischemia and hypoxia can cause widespread myocardial degeneration and fibrosis, leading to ventricular dilation and the development of ischemic cardiomyopathy. This condition is characterized primarily by heart failure and is associated with a poor prognosis.
Treatment
The treatment of CAD can be classified into three main approaches: medical therapy, interventional therapy, and surgical therapy. The choice of treatment depends on the specific condition of the patient, with the aim of alleviating symptoms, improving quality of life, and prolonging survival.
Surgical Treatment
Surgical treatment for CAD predominantly involves coronary artery bypass grafting (CABG), which reconstructs blood flow to ischemic myocardium to improve myocardial oxygenation and perfusion.
Indications for surgical treatment mainly include angina that interferes with daily activities and is unresponsive to medical therapy. CABG is often considered for patients with significant narrowing of the main coronary artery or major branches, as identified by coronary angiography, where blood flow distal to the narrowing remains unobstructed. Early surgery is typically recommended for patients with severe left main coronary artery stenosis or proximal stenosis of the left anterior descending (LAD) artery due to the increased risk of sudden cardiac death. Indications also include proximal LAD artery stenosis combined with significant narrowing of the circumflex artery and/or right coronary artery, myocardial ischemia demonstrated through functional testing, left ventricular dysfunction, or coexisting diabetes mellitus.
Prior to CABG, selective coronary angiography is performed to precisely identify the location and severity of the atherosclerotic lesions, assess the condition of distal coronary blood flow, and evaluate left ventricular function.
CABG often involves revascularizing multiple stenotic coronary arteries. Common techniques include an end-to-side anastomosis of the internal thoracic artery to a distal coronary artery branch beyond the stenosis. Alternatively, a segment of autologous great saphenous vein can be used for anastomosis, with the proximal (heart-facing) and distal (downstream) ends connected to the ascending aorta and the distal coronary branch beyond the stenosis, respectively. A single great saphenous vein or radial artery may also be used for sequential or snake-like end-to-side and side-to-side anastomoses to multiple stenotic vessels.

Figure 1 End-to-side anastomosis of internal thoracic artery to left coronary artery
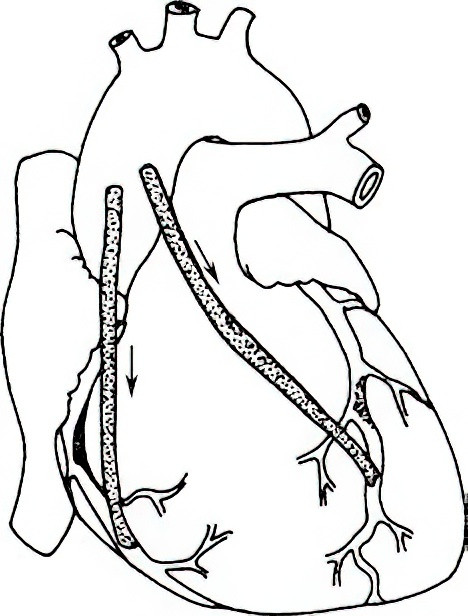
Figure 2 Saphenous vein graft from ascending aorta to coronary artery
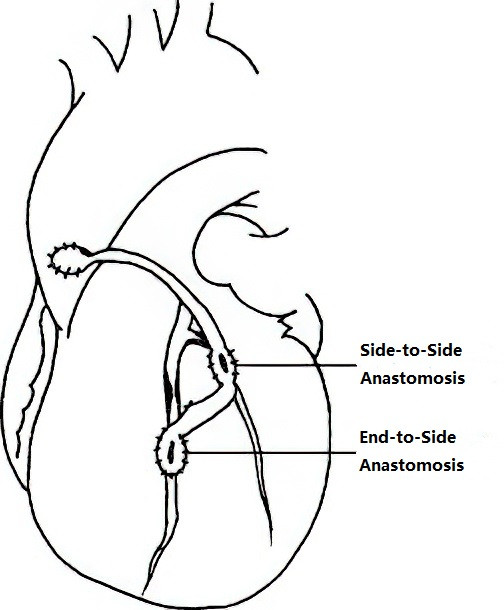
Figure 3 Sequential anastomosis
CABG is typically performed with the assistance of cardiopulmonary bypass (CPB), allowing the surgery to be completed on a non-beating heart. However, off-pump coronary artery bypass techniques have become available through the use of specialized stabilizers affixed to the heart surface. Off-pump CABG avoids the use of CPB, reducing the impact on the hematologic system, lungs, kidneys, and other organs, as well as minimizing perioperative blood transfusion requirements. Nonetheless, off-pump CABG is more technically demanding and may result in incomplete revascularization, potentially affecting long-term outcomes.
Among bypass grafts, the internal thoracic artery has the highest long-term patency rate, followed by the radial artery and the great saphenous vein. Recent advancements in percutaneous coronary stent materials have improved stent patency rates to levels comparable to those of venous grafts. As a result, hybrid techniques combining minimally invasive internal thoracic artery-LAD bypass with stent implantation for non-LAD lesions have emerged as personalized approaches for complex multivessel disease.
Surgical treatment is also applicable to complications of myocardial infarction, such as ventricular aneurysm, ventricular septal perforation, and mitral regurgitation due to papillary muscle or chordae tendineae rupture. CABG can be performed concurrently as needed. In cases of advanced ischemic cardiomyopathy, marked ventricular dilation, or refractory heart failure, further options such as ventricular assist devices or heart transplantation may be considered.