Echinococcosis is a parasitic disease common in pastoral regions. Most cases are caused by the larval stage of Echinococcus granulosus, which forms cysts in organs such as the liver and lungs, leading to various complications. This condition is also referred to as hydatid disease. Pulmonary echinococcosis accounts for about 10%–15% of echinococcosis cases, typically presenting as solitary cysts that are more frequently observed in the right lung compared to the left lung, and in the lower lobes compared to the upper lobes.
Clinical Manifestations
Due to the slow growth of pulmonary echinococcal cysts, asymptomatic periods can last for years if complications are absent. Once cysts enlarge, symptoms such as cough, chest pain, hemoptysis, and dyspnea may develop. When cyst rupture occurs into the bronchus, it can cause paroxysmal coughing followed by expectoration of large amounts of clear mucus, and in some cases, the detached inner cyst may be expelled, revealing Echinococcus scolices in the sputum. Secondary infections present symptoms similar to a lung abscess, including fever, purulent sputum, and hemoptysis.
If the cyst ruptures into the pleural cavity, it can lead to hydropneumothorax, later progressing to empyema. In certain cases, hypersensitivity reactions such as rash, fever, nausea, vomiting, abdominal pain, bronchospasm, and shock may occur, with severe cases potentially being fatal. Large cysts can compress the mediastinum, resulting in displacement of the trachea or heart.
Diagnosis
The diagnosis of pulmonary echinococcosis is typically based on the following:
Epidemiological History
Cases often involve patients who live in or have visited areas endemic for echinococcosis, with a history of exposure to domestic animals such as dogs, sheep, cattle, or horses.
Imaging Findings on Chest X-Ray or CT
Uncomplicated cysts typically appear as solitary or multiple round or oval lesions with uniform density, clearly defined margins, and smooth edges.
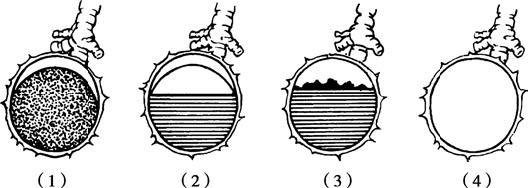
Figure 1 Various radiological signs of ruptured pulmonary hydatid cysts
(1) Outer cyst rupture showing crescent-shaped translucency at the top.
(2) Rupture of both inner and outer cysts with fluid-air level and double curved translucent bands.
(3) Inner cyst collapse floating in fluid, resembling the "water lily sign."
(4) Complete rupture with evacuated contents, forming a cystic translucency resembling a pulmonary bulla.
Signs associated with ruptured cysts include:
- Outer cyst rupture: A crescent-shaped radiolucent area appears at the top of the cyst due to air entering the space between the inner and outer cyst walls.
- Rupture of both inner and outer cysts: Partial evacuation of cyst fluid and simultaneous entry of air creates a fluid-air level with two curved radiolucent bands above it.
- Collapsed cyst floating in the remaining cyst fluid: An irregular floating opacity resembling a "water lily sign" is visible above the fluid line.
- Complete rupture and evacuation of contents: A cystic radiolucent opacity similar to a pulmonary bulla is observed.
Laboratory Investigation
Blood tests often reveal elevated eosinophil counts, sometimes reaching 25%–30%. Diagnostic tests such as complement fixation for Echinococcus antigens and the Casoni intradermal test yield positive results, with sensitivity rates of 70%–90%.
Pulmonary echinococcosis should not be diagnosed using needle aspiration procedures, as this may lead to leakage of cyst fluid, causing allergic reactions or dissemination of Echinococcus larvae with serious complications.
Prevention
Preventive measures in endemic regions include public health education emphasizing food and water hygiene, proper handwashing before meals, and safeguarding water sources. Epidemiological surveys are necessary to monitor disease prevalence, and control measures such as deworming of livestock dogs and stricter management of slaughterhouses can reduce the incidence rate.
Treatment
Currently, there is no specific pharmacological treatment for echinococcosis; surgical intervention remains the only effective method for treating pulmonary echinococcal cysts. The procedure involves complete removal of the inner cyst while preventing leakage of cyst fluid to avoid allergic reactions or dissemination of echinococcal larvae. The following surgical methods are available:
Cystectomy (Inner Cyst Removal)
This method is suitable for uncomplicated pulmonary echinococcal cysts. During surgery, spillage of cyst fluid into surrounding tissues must be avoided to prevent allergic reactions. Some fluid may be aspirated using a needle, and a small amount of 10% saline solution can be injected to sterilize the scolices. After 15 minutes, the surgeon incises the outer cyst and removes the inner cyst completely and intact. Alternatively, the cyst may be left unpunctured; the plane of separation between the outer and inner cyst walls is widened, and inflation of the lung through positive pressure ventilation facilitates complete removal of the inner cyst. The outer cyst wall is peeled and excised, and fine sutures are used to close any small bronchial openings.
Cyst Excision
This technique is used for smaller, uncomplicated cysts located deep within lung tissue. Both the inner and outer cyst walls are removed together, and the lung tissue defect is sutured.
Lobectomy or Segmentectomy
This method is indicated when the cyst has caused secondary infections, leading to pathological changes in the surrounding lung tissue.