Pneumothorax refers to the accumulation of air in the pleural cavity. It may result from the rupture of pulmonary bullae, though it occurs more frequently due to trauma, surgical procedures, positive-pressure mechanical ventilation, thoracentesis, or the insertion of cardiac or vascular catheters. Such events can cause ruptures in the lungs, trachea, bronchi, or esophagus, allowing air to escape into the pleural cavity. Alternatively, it may occur when chest wall injuries perforate the pleura, establishing communication between the pleural cavity and the external environment, permitting the entry of external air. Pneumothorax is classified into three types: closed pneumothorax, open pneumothorax, and tension pneumothorax. Free air within the pleural cavity accumulates in the upper section of the thoracic cavity depending on the patient’s positioning. Adhesions in the pleural cavity caused by inflammation or surgical intervention can localize the pneumothorax to certain regions, forming a localized pneumothorax.
Closed Pneumothorax
Closed pneumothorax occurs when chest wall wounds are sealed or lung lacerations are small. As the volume of intrapleural air and the degree of lung collapse increase, the laceration on the lung surface may contract, eventually failing to reopen even during inspiration. In such cases, the pneumothorax stabilizes and may be slowly reabsorbed. The extent of lung collapse on the affected side depends on the volume of air in the pleural cavity. Reduced lung participation leads to decreased respiratory surface area, ventilation-perfusion mismatches, and impaired respiratory gas exchange. The increased intrathoracic pressure on the affected side may cause mediastinal shift toward the healthy side. Depending on the volume and rate of air accumulation in the pleural cavity, patients may be asymptomatic in mild cases or exhibit significant dyspnea in severe cases. Physical examination may reveal fullness of the chest wall on the affected side, reduced respiratory movement, tracheal deviation toward the healthy side, tympanic resonance on percussion, and diminished breath sounds on auscultation. Chest X-rays or CT scans may show varying degrees of lung collapse and pleural air accumulation, sometimes accompanied by small amounts of pleural effusion.
Patients with slow-onset pneumothorax and small air volumes may recover without specialized intervention, as the entrapped air typically reabsorbs within one to two weeks. In cases of large pneumothorax, thoracentesis or thoracic closed drainage may be necessary to remove air from the pleural cavity and facilitate lung re-expansion.
Open Pneumothorax
Open pneumothorax occurs when air freely enters and exits the pleural cavity through a chest wall wound or soft tissue defect during respiration. The air volume exchanged depends on the size of the chest wall wound. If the wound is larger than the tracheal diameter, significant air flows into the pleural cavity, causing intrathoracic pressure to equalize with atmospheric pressure. This leads to complete lung collapse and loss of respiratory function on the affected side. The increased intrathoracic pressure compared to the healthy side further restricts contralateral lung expansion. Periodic pressure changes between the two pleural cavities during respiration result in mediastinal flutter, a phenomenon where the mediastinum shifts toward the healthy side during inspiration and returns to the injured side during expiration. Such oscillation and displacement impair venous return to the heart, potentially causing severe circulatory dysfunction.
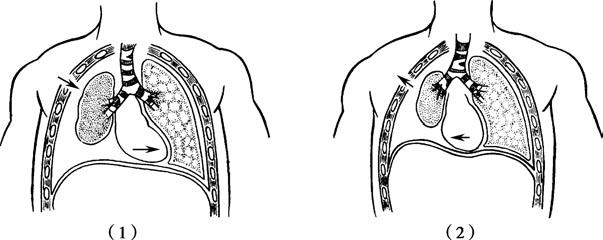
Figure 1 Mediastinal flutter in open pneumothorax
(1) During Inspiration (2) During Expiration
Patients may present with pronounced dyspnea, nasal flaring, cyanosis of the lips, and distended jugular veins. Chest wall wounds on the affected side may produce a sucking sound as air moves in and out of the pleural cavity, which is referred to as a sucking chest wound. Tracheal deviation toward the healthy side, tympanic resonance upon percussion, and absent breath sounds on auscultation are observed, and severe cases may progress to shock. Chest X-rays may reveal a large volume of intrapleural air, complete lung collapse, and mediastinal shift to the healthy side.
Emergency management of open pneumothorax includes sealing the chest wall wound to create a closed pneumothorax and buying time for life-saving interventions until patients can be transported to a medical facility. Sterile materials such as Vaseline gauze, cotton pads, or clean items including plastic bags, clothing, or cups can be used to create airtight dressings. These materials are applied to the wound at the end of forced expiration, followed by pressure dressing. If the patient's respiratory distress worsens or signs of tension pneumothorax develop during transport, the sealed dressing may be temporarily released during expiration to allow decompression of high-pressure gas. Thoracic closed drainage should be performed when conditions permit. Hospital management involves oxygen supplementation, volume resuscitation, and shock correction. Procedures include wound debridement, chest wall suturing, and placement of a thoracic closed drainage tube. The administration of antibiotics and encouragement of coughing to clear secretions are recommended to prevent infections. Persistent or worsening pneumothorax, suspected thoracic organ injury, or progressive bleeding may require thoracotomy for exploration.
Chest closed drainage indications include:
- Moderate or large-volume closed pneumothorax, open pneumothorax, or tension pneumothorax.
- Failure of lung re-expansion after thoracentesis.
- Pneumothorax or hemopneumothorax requiring mechanical or artificial ventilation.
- Recurrent pneumothorax or hemothorax after removal of the drainage tube.
- Post-thoracotomy cases.
The placement site for the drainage tube is determined based on clinical findings. Pneumothorax drainage typically involves the second intercostal space along the midclavicular line, while hemothorax is drained at the sixth or seventh intercostal space between the midaxillary and posterior axillary lines. After local sterilization, local anesthesia infiltrates all layers of the chest wall. The skin is incised, muscle layers are bluntly separated, and a chest drainage tube with side holes is inserted above the rib margin.

Figure 2 Thoracic closed drainage procedure
The side holes of the drainage tube are positioned 2–3 cm inside the pleural cavity. The drainage tube is connected to a closed drainage system to allow air or fluid to drain at pressures exceeding 3–4 cmH2O while preventing the entry of external air or fluid. Drainage tube function is monitored by frequent observation, and the volume of air and fluid drainage is recorded hourly or over 24 hours. If the lung re-expands well and there is no further drainage, the tube can be removed during deep inspiration with breath-holding, followed by closure of the wound.
Tension Pneumothorax
Tension pneumothorax refers to a condition in which a one-way valve is formed at the site of injury to the trachea, bronchus, or lung, allowing air to continuously enter the pleural cavity with each breath but preventing its escape. This leads to progressive accumulation of air within the pleural cavity, causing intrapleural pressure to rise above atmospheric pressure. It is also referred to as high-pressure pneumothorax. The affected lung undergoes severe collapse, the mediastinum shifts markedly toward the healthy side, and compression of the contralateral lung occurs, along with impaired venous return to the heart. Elevated intrathoracic pressure drives air through bronchial or tracheal connective tissue planes or ruptures in the parietal pleura into the mediastinum or chest wall soft tissues, resulting in mediastinal emphysema or subcutaneous emphysema in the face, neck, and chest.
Patients with tension pneumothorax typically exhibit severe or extreme respiratory distress, restlessness, altered consciousness, profuse sweating, and cyanosis. Significant tracheal deviation toward the healthy side, jugular vein distension, and subcutaneous emphysema are commonly observed. The affected side of the chest may appear distended, percussion reveals hyper-resonance, and breath sounds are absent. Chest X-rays reveal extensive air accumulation in the pleural cavity, complete lung collapse, mediastinal shift, and possibly mediastinal and subcutaneous emphysema. Thoracentesis in such cases often ejects high-pressure air that forces the syringe plunger outward. Critically ill patients may develop signs of circulatory compromise, such as a rapid thready pulse and reduced blood pressure. Tension pneumothorax is a life-threatening emergency capable of causing rapid death.
Emergency management before and during hospitalization involves prompt pleural cavity decompression using a large-bore needle connected to a one-way valve device. In urgent situations, surgical gloves, soft plastic bags, or balloons punctured with small openings can be attached to the needle hub to allow the high-pressure air in the pleural cavity to escape while preventing external air from entering. Subsequent treatment includes the placement of a thoracic closed drainage system and the administration of antibiotics to prevent infections. The closed drainage system can be further connected to negative-pressure suction devices to expedite air evacuation and facilitate lung re-expansion. The drainage tube is removed only after air leakage has ceased for 24 hours, and chest X-rays confirm complete lung re-expansion. Persistent air leaks or an inability to achieve lung re-expansion necessitate thoracotomy or video-assisted thoracoscopic surgery for further exploration.