Phyllodes tumor (PT) is a fibroepithelial neoplasm of the breast composed of both epithelial and stromal components. It accounts for approximately 0.3%–1% of all breast tumors, with a higher incidence reported among Asian women compared to European women.
Pathological Classification
Based on histopathological features such as tumor margins, stromal cell density, cellular atypia, mitotic activity, stromal overgrowth, and the presence of malignant heterologous components, the World Health Organization (WHO) classifies phyllodes tumors into three categories: benign, borderline, and malignant. The degree of malignancy increases with a higher proportion of stromal components and a lower proportion of epithelial components.
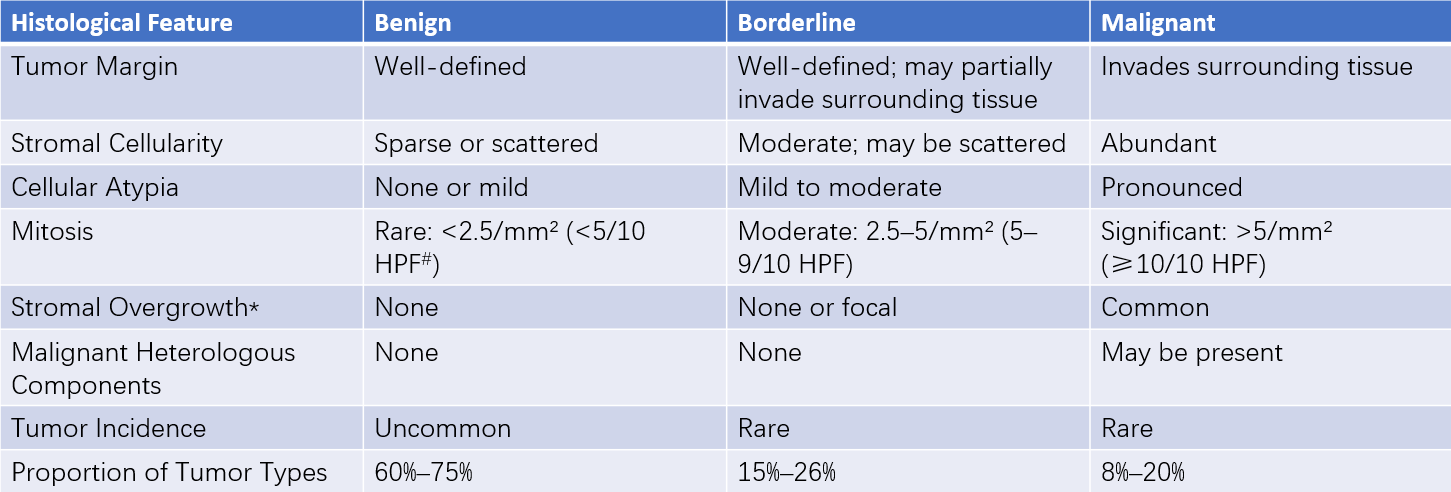
Table 1 Histological features of WHO classification of phyllodes tumors (5th edition, WHO)
Notes:
#HPF refers to high-power field in microscopy.
*Stromal overgrowth is defined as the absence of epithelial components in a single low-power field.
Clinical Manifestations
This condition typically occurs in women aged 40–50 and presents as a solitary, relatively large, well-mobile mass. Rapid growth of the mass may occur over a short period. Larger tumors may lead to thinning and shiny appearance of the overlying breast skin, and in severe cases, ulceration or necrosis may develop. Physical examination often reveals a rounded, lobulated, and smooth-surfaced mass, while axillary lymphadenopathy is rarely observed.
Treatment
Surgery represents the primary mode of treatment. For benign phyllodes tumors, tumor excision is performed, whereas borderline and malignant phyllodes tumors require wide excision with tumor-free margins of more than 1 cm. Phyllodes tumors generally show poor responsiveness to radiotherapy or chemotherapy.
Prognosis
Phyllodes tumors exhibit a high rate of local recurrence, with recurrence rates of 10%–17% for benign tumors, 14%–25% for borderline tumors, and 23%–30% for malignant tumors. Recurrent tumors often show progression in their histological grade. Malignant phyllodes tumors have the potential for hematogenous metastasis, with a reported metastasis rate of up to 25%. The lungs and bones are the most common sites of metastasis, while axillary lymph node involvement is relatively rare.