Acute mastitis is an acute suppurative infection of the breast, commonly occurring in women during the postpartum breastfeeding period. It is most frequently seen in primiparous women, with onset typically occurring 3 to 4 weeks after delivery.
Etiology
The condition is caused by milk stasis and bacterial invasion. The primary causative pathogen is Staphylococcus aureus.
Clinical Manifestations
Symptoms include breast pain, localized redness and swelling, and fever. As the inflammation progresses, additional symptoms such as chills, high fever, tachycardia, and enlargement or tenderness of the axillary lymph nodes on the affected side may occur. Laboratory findings often show significant elevations in white blood cell count, neutrophil count, and C-reactive protein levels.
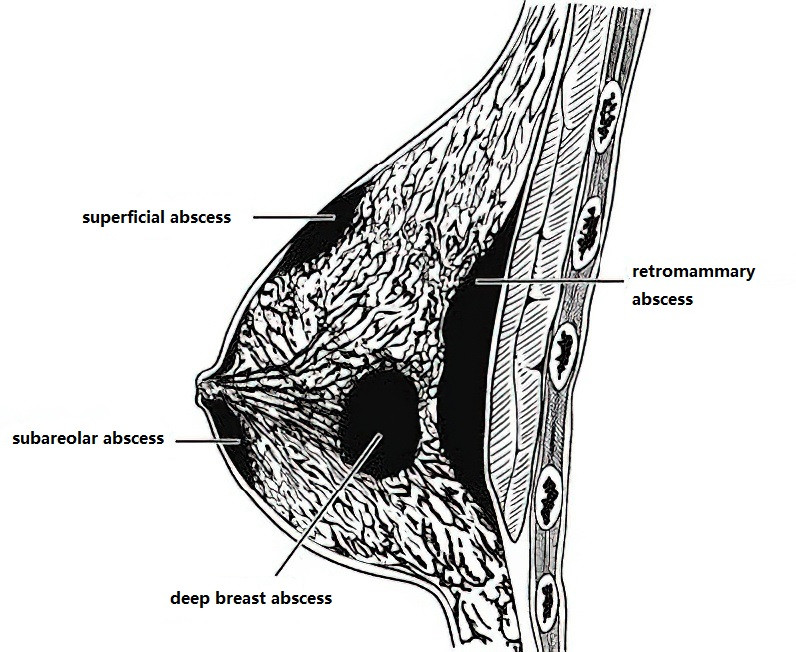
Figure 1 Locations of breast abscesses
Severe inflammation may lead to the formation of a breast abscess. Superficial abscesses may present with palpable fluctuation, while deeper abscesses require ultrasound examination or aspiration of pus for confirmation. Abscesses may be unilocular or multilocular. An abscess can rupture externally or extend into the loose tissues between the breast and pectoral muscles, leading to the formation of a retromammary abscess. In severe cases, sepsis may develop as a complication.
Treatment
The primary treatment principles involve emptying the breast of milk and resolving the infection.
In the absence of abscess formation, early administration of antibiotics is effective. Since Staphylococcus aureus is the most common pathogen, empirical treatment with penicillin can be administered. For patients allergic to penicillin, erythromycin may be used as an alternative. Medications such as tetracyclines, aminoglycosides, quinolones, sulfonamides, and metronidazole should be avoided to prevent harm to the infant from drug transmission through breast milk.
If an abscess has developed, aspiration of the abscess should be performed, and pus should undergo bacterial culture and sensitivity testing to guide the selection of antibiotics.
For larger or multilocular abscesses, surgical incision and drainage are necessary. To minimize the risk of damaging milk ducts and causing mammary fistula, the incision should be made at the lowest point of the abscess. For abscesses beneath the areola, a curved incision along the edge of the areola is preferred. Deep or retromammary abscesses can be drained via a curved incision along the lower edge of the breast, entering through the retromammary space. Multilocular abscesses should be gently separated with a finger during surgery to ensure adequate drainage.
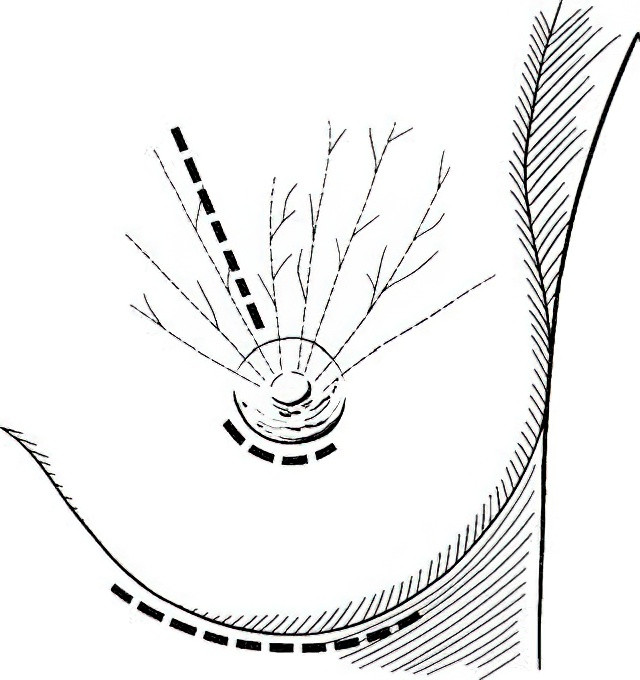
Figure 2 Incisions for draining breast abscesses
Prevention
Prevention of the condition involves avoiding milk stasis, protecting the nipple from injury, and maintaining cleanliness. For mild inflammation, breastfeeding from the unaffected breast may continue, while breastfeeding from the affected breast should cease, with milk being expressed using a breast pump to ensure proper drainage. In cases of severe infection or complications such as mammary fistula after abscess drainage, breastfeeding should be stopped. Suppression of lactation may involve oral administration of bromocriptine or diethylstilbestrol, or intramuscular injection of estradiol benzoate.