Thyroid carcinoma is the most common malignant tumor of the endocrine system, accounting for approximately 1% of all malignant tumors. The incidence rate has been increasing in recent years.
Pathology
Papillary Carcinoma
Papillary carcinoma is the most common pathological type of thyroid cancer in both adults and children, primarily affecting women aged 30 to 50 years. It has a high degree of differentiation and low malignancy. Although often presenting with multifocal lesions and early cervical lymph node metastasis, the prognosis is generally favorable.
Follicular Carcinoma
Follicular carcinoma is more common among women aged 40 to 60 years. It tends to grow faster and has a propensity for vascular invasion. Cervical lymph node metastasis occurs in only about 10% of cases, but hematogenous spread to organs such as the lungs and bones is common, resulting in a prognosis that is less favorable than that of papillary carcinoma. Papillary carcinoma and follicular carcinoma are collectively referred to as differentiated thyroid carcinoma, which accounts for more than 90% of adult thyroid cancers.
Medullary Carcinoma
Medullary carcinoma originates from parafollicular (C) cells, which secrete calcitonin. It exhibits moderate malignancy and may involve both cervical lymph node and hematogenous metastasis. While the prognosis is not as good as that of differentiated thyroid carcinoma, it is better than that of undifferentiated carcinoma.
Undifferentiated Carcinoma
Undifferentiated carcinoma often develops in elderly individuals around the age of 70. It progresses rapidly and is highly malignant. Approximately 50% of patients present with cervical lymph node metastasis at an early stage. It frequently invades surrounding tissues and metastasizes to distant organs such as the lungs and bones. The prognosis is poor, with an average survival of 3 to 6 months and a 1-year survival rate of only 5% to 15%.
Clinical Manifestations
In the early stages, thyroid carcinoma often manifests as an asymptomatic nodule, most of which are discovered incidentally during routine physical examination. A small number of cases present initially with cervical lymphadenopathy. As the disease progresses, the tumor may compress or invade structures such as the trachea, esophagus, and nerves, leading to symptoms such as breathing difficulty, swallowing difficulty, and hoarseness. Advanced stages may involve metastasis to distant organs such as the lungs and bones, resulting in corresponding clinical presentations. In some cases, patients may present without obvious thyroid enlargement but seek medical attention due to metastatic lesions, raising suspicion of thyroid carcinoma.
For medullary carcinoma, in addition to neck masses, symptoms such as diarrhea, facial flushing, and excessive sweating may occur, as the tumor can produce calcitonin, prostaglandins, serotonin, and other substances.
Diagnosis
Neck ultrasound is one of the key auxiliary diagnostic methods. Fine-needle aspiration biopsy is an important method for preoperative diagnosis of thyroid nodules or suspicious lymph nodes. Factors such as a firm and fixed thyroid mass, cervical lymphadenopathy, or a long-term thyroid lesion that enlarges rapidly over a short period raise suspicion of thyroid carcinoma. Additionally, serum calcitonin measurement can assist in diagnosing medullary carcinoma.
Clinical Staging
In the 2017 edition of the American Joint Committee on Cancer (AJCC) TNM staging system for thyroid carcinoma, greater emphasis is placed on the degree of tumor invasion, pathological type, and age at diagnosis.
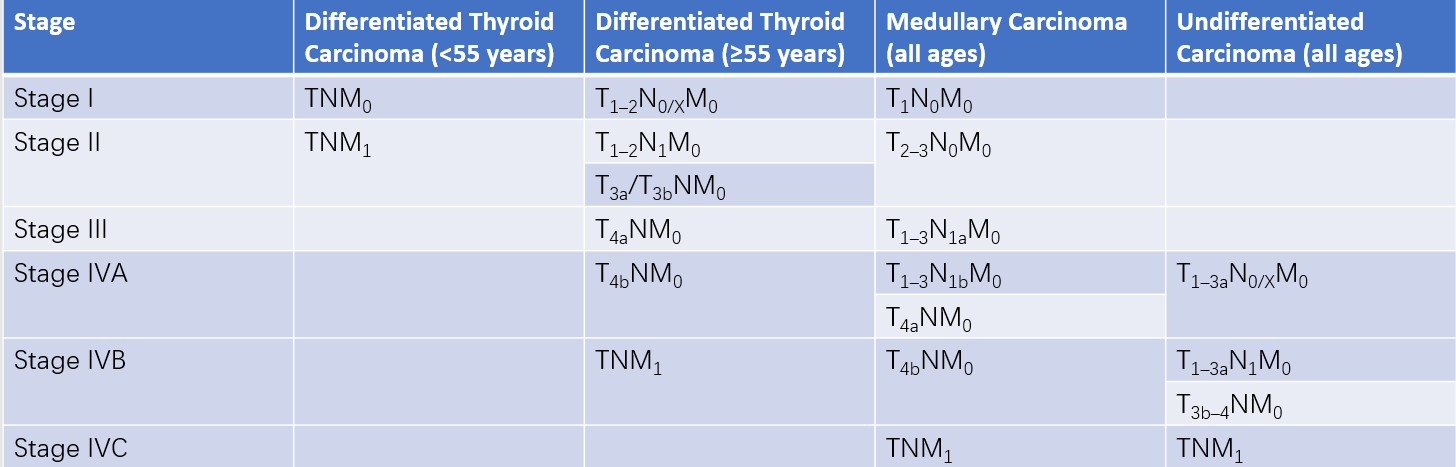
Table 1 Clinical staging of thyroid cancer
T (Primary Tumor)
TX: Primary tumor cannot be assessed.
T0: No evidence of a primary tumor.
T1: Tumor ≤2 cm in greatest dimension and confined to the thyroid.
T1a: Tumor ≤1 cm in greatest dimension and confined to the thyroid.
T1b: Tumor >1 cm but ≤2 cm in greatest dimension and confined to the thyroid.
T2: Tumor >2 cm but ≤4 cm in greatest dimension and confined to the thyroid.
T3: Tumor >4 cm in greatest dimension and confined to the thyroid; or any tumor with gross extrathyroidal extension limited to strap muscles.
T3a: Tumor >4 cm in greatest dimension and confined to the thyroid.
T3b: Tumor of any size with gross extrathyroidal extension into strap muscles (including sternohyoid, sternothyroid, thyrohyoid, or omohyoid muscles).
T4: Tumor with gross extrathyroidal extension beyond the strap muscles.
T4a: Tumor of any size with gross extrathyroidal extension to subcutaneous soft tissue, larynx, trachea, esophagus, or recurrent laryngeal nerve.
T4b: Tumor of any size with gross extrathyroidal extension to prevertebral fascia, encasement of carotid artery, or mediastinal vessels.
N (Regional Lymph Nodes)
NX: Regional lymph nodes cannot be assessed.
N0: No evidence of regional lymph node metastasis.
N1: Regional lymph node metastasis.
N1a: Metastasis to lymph nodes in level VI or VII (pretracheal, paratracheal, Delphian lymph nodes, or superior mediastinal lymph nodes), which may be unilateral or bilateral.
N1b: Metastasis to unilateral, bilateral, or contralateral cervical lymph nodes (levels I, II, III, IV, or V) or retropharyngeal lymph nodes.
M (Distant Metastasis)
M0: No distant metastasis.
M1: Presence of distant metastasis.
For differentiated thyroid carcinoma, which progresses relatively slowly and is associated with long survival times, the American Thyroid Association has introduced an initial risk stratification system based on clinical and pathological features obtained during surgery. This stratification divides patients into low, intermediate, and high-risk categories to guide postoperative clinical decision-making.
Treatment
Except for undifferentiated carcinoma, surgical intervention remains the primary treatment for other types of thyroid carcinoma, supplemented by therapies such as TSH suppression, radionuclide therapy, and external radiation therapy.
Surgical Treatment
Surgery plays a critical role in the management of thyroid carcinoma. The surgical approach varies depending on the pathological type and extent of tumor invasion. Surgical interventions primarily include thyroid resection and cervical lymph node dissection.
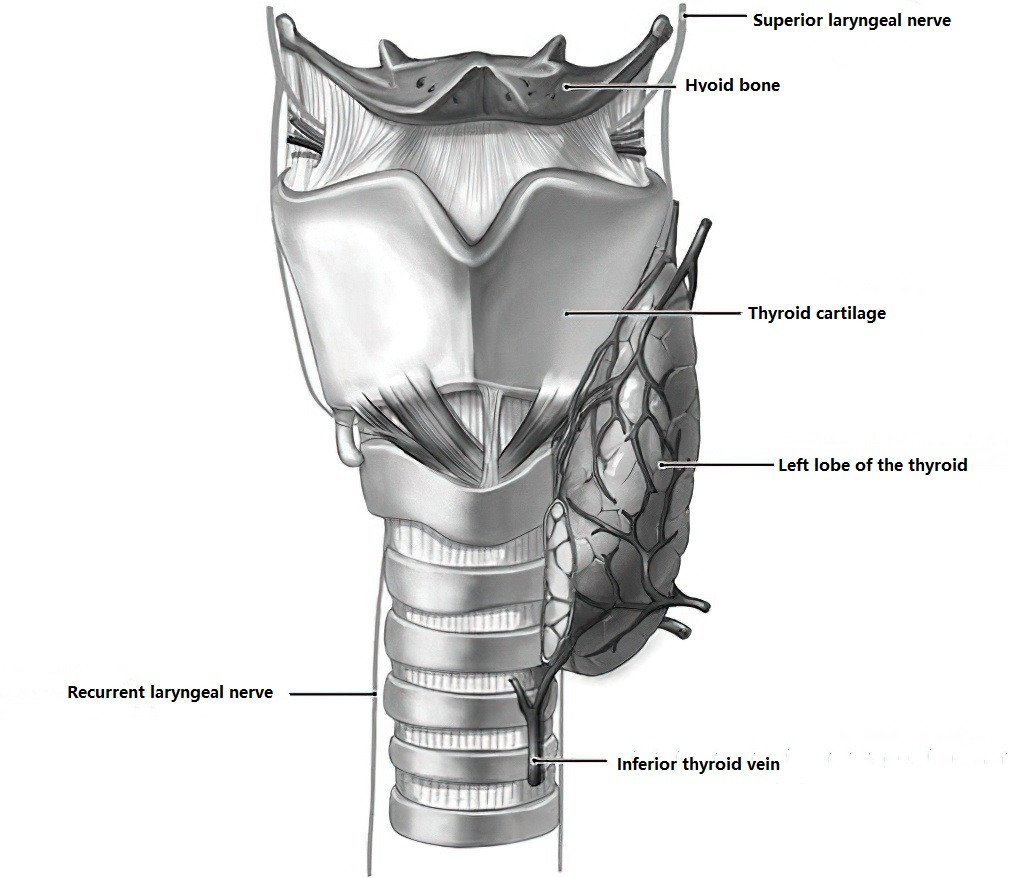
Figure 1 Postoperative schematic diagram of right thyroid lobe and isthmus resection
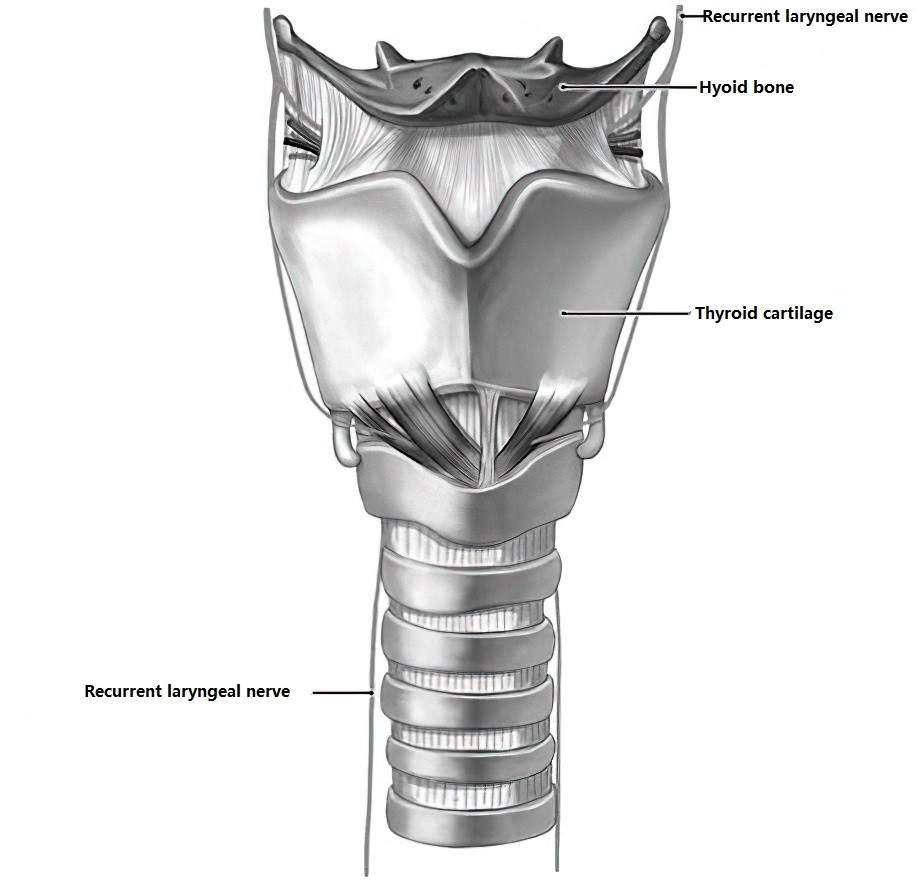
Figure 2 Postoperative schematic diagram of total thyroidectomy
For differentiated thyroid carcinoma, there is ongoing debate about the extent of thyroid resection, but consensus has been reached that the minimum required extent is lobectomy (including the isthmus). Total or near-total thyroidectomy is recommended for patients with diagnosed differentiated thyroid carcinoma who meet any of the following criteria:
- A history of cervical radiation exposure
- Presence of distant metastases
- Bilateral cancerous nodules
- Macroscopic extrathyroidal extension
- Tumor diameter >4 cm
- Poor prognostic pathological subtypes, such as tall cell or columnar cell variants
- Extensive bilateral cervical lymph node metastasis
Lobectomy (including the isthmus) is recommended only for patients who fulfill all of the following criteria:
- No history of cervical radiation exposure
- No evidence of distant metastases
- No extrathyroidal extension
- Absence of poor prognostic pathological variants
- No evidence of clinically significant lymph node metastasis
- Tumor diameter <1 cm
For tumors measuring 1–4 cm in diameter, relative high-risk factors should be thoroughly evaluated, and the surgical approach should be determined in consultation with the patient's preferences. Total or near-total thyroidectomy is generally recognized as the most effective treatment method for medullary thyroid carcinoma.
Regarding cervical lymph node dissection, consensus has been reached within domestic practice to perform at least ipsilateral central compartment lymph node dissection during surgery for all patients with differentiated thyroid carcinoma, ensuring effective protection of the parathyroid glands and the recurrent laryngeal nerve. Central compartment dissection targets the area most prone to metastasis and contributes to accurate clinical staging, guiding treatment decisions and reducing complications associated with reoperation. Prophylactic lateral cervical lymph node dissection is usually not performed. Therapeutic lateral cervical lymph node dissection is carried out only for patients with confirmed metastasis based on preoperative biopsy findings, imaging studies, or intraoperative frozen pathology. In cases without organ involvement, modified lateral cervical lymph node dissection (zones II–V) is typically performed, preserving the sternocleidomastoid muscle, internal jugular vein, and accessory nerve.
TSH Suppression Therapy
TSH suppression therapy is designed to inhibit TSH secretion postoperatively in patients with differentiated thyroid carcinoma to suppress the growth of cancerous tissues. Optimal target levels aim to reduce the rates of recurrence, metastasis, and cancer-related mortality while minimizing adverse reactions associated with exogenous subclinical hyperthyroidism.
For patients with varying risks of recurrence, different degrees of TSH suppression therapy are applied, with adjustments to medication dosage and duration based on the patient's risks of adverse reactions and therapeutic outcomes (dual risk assessment).
Generally, during the initial treatment phase, patients stratified as high-risk require TSH suppression below 0.1 mU/L; for intermediate-risk patients, suppression between 0.1 and 0.5 mU/L is recommended; and for low-risk patients, suppression between 0.5 and 2 mU/L is advised. Dose adjustments and dynamic evaluations are carried out based on adverse reactions and efficacy. Lifetime suppression is typically suggested for intermediate- and high-risk patients. Low-risk patients may undergo suppression therapy for 5 to 10 years, after which replacement therapy is provided.
Radionuclide Therapy
Both normal thyroid tissue and cells of differentiated thyroid carcinoma exhibit an ability to uptake iodine-131 (131I). This property is leveraged to deliver ionizing radiation from beta emissions of 131I to destroy residual thyroid tissue or cancer cells, thereby achieving therapeutic outcomes.
The goals of 131I therapy include:
- Ablative treatment: Removal of residual thyroid tissue following thyroid carcinoma surgery.
- Adjuvant treatment: Elimination of potentially microscopic metastatic or residual lesions that are undetectable with imaging.
- Targeted treatment: Treatment of documented local or distant metastatic lesions that cannot be surgically removed.
Ablative removal of residual thyroid tissue reduces the likelihood of recurrence and metastasis. Once residual thyroid tissue is fully ablated, elevated TSH levels enhance the iodine uptake ability of metastatic lesions, facilitating 131I imaging and subsequent therapeutic intervention for metastases.
External Radiation Therapy
External radiation therapy is primarily indicated for undifferentiated thyroid carcinoma.