Tethered cord syndrome (TCS) refers to pathological conditions where the spinal cord or its conus medullaris is subjected to traction due to congenital or acquired factors. This traction results in ischemia, hypoxia, and degeneration of neural tissue, causing a series of neurological symptoms and signs such as pain in the lumbosacral region or legs, as well as motor and sensory disturbances. The condition is most commonly seen in infants, young children, and adolescents, with a higher prevalence among females than males. TCS typically progresses slowly and often involves the lumbosacral spinal cord, leading to an abnormally low positioning of the conus medullaris in many cases.
Clinical Manifestations
Abnormal Lumbosacral Skin
Characteristic skin abnormalities are frequently observed. Ninety percent of affected children present with subcutaneous masses. Fifty percent may exhibit skin dimples, meningocele, vascular malformations, or hypertrichosis (excessive hair growth).
Pain
Pain is the most common symptom. It is typically diffuse and lacks a dermatome-specific distribution. The pain may be unilateral or bilateral radiating pain. In children, pain is often localized to the lumbosacral region and may radiate to the lower limbs. In adults, pain is more widespread and may involve the deep anal and rectal regions, the middle of the buttocks, the perineum, the lower limbs, and the lower back.
Bladder and Rectal Dysfunction
Bladder and rectal symptoms are commonly seen together. Bladder dysfunction may include bedwetting, urinary frequency, urgency, incontinence, or retention. Rectal issues may manifest as constipation or fecal incontinence. In children, bedwetting and urinary incontinence are the most common presentations.
Sensory Impairment
Numbness or reduced sensation often occurs in the saddle region and distal lower limb skin. Skin ulcers may also develop in these areas.
Motor Dysfunction
Progressive weakness in one or both lower limbs and difficulty walking are commonly observed motor impairments.
Musculoskeletal Abnormalities
Foot deformities are the most frequent musculoskeletal features. These may include foot asymmetry, high-arched clubfoot, claw toes, and dystrophic ulcers.
Auxiliary Testing
MRI
MRI is the optimal and preferred diagnostic tool, capable of clearly demonstrating the position and morphology of the conus medullaris, as well as revealing any thickened filum terminale. MRI can also detect conditions such as intraspinal (or extraspinal) lipomas, teratomas, syringomyelia, split cord malformations, and other abnormalities.
CT
CT imaging is useful in visualizing bone deformities such as spina bifida.
X-ray Imaging
X-rays are primarily employed to assess for scoliosis and to guide preoperative vertebral localization.
Other Tests
Additional diagnostic tools include neuroelectrophysiological tests, ultrasound, and bladder function assessments, which are instrumental for diagnosis and evaluation of postoperative functional status.
Diagnosis
Diagnosis requires a combination of clinical presentation and radiological evaluations. Common diagnostic clues include widespread pain that cannot be explained by damage to a single nerve, adult-onset symptoms with evident triggers, bladder and rectal dysfunction often complicated by urinary tract infections, progressively worsening sensory and motor disturbances, congenital anomalies, and a history of prior lumbar surgery. MRI and/or CT myelography may reveal abnormal positioning of the conus medullaris or a thickened filum terminale. Early symptoms may be covert, making diagnosis challenging in some cases.
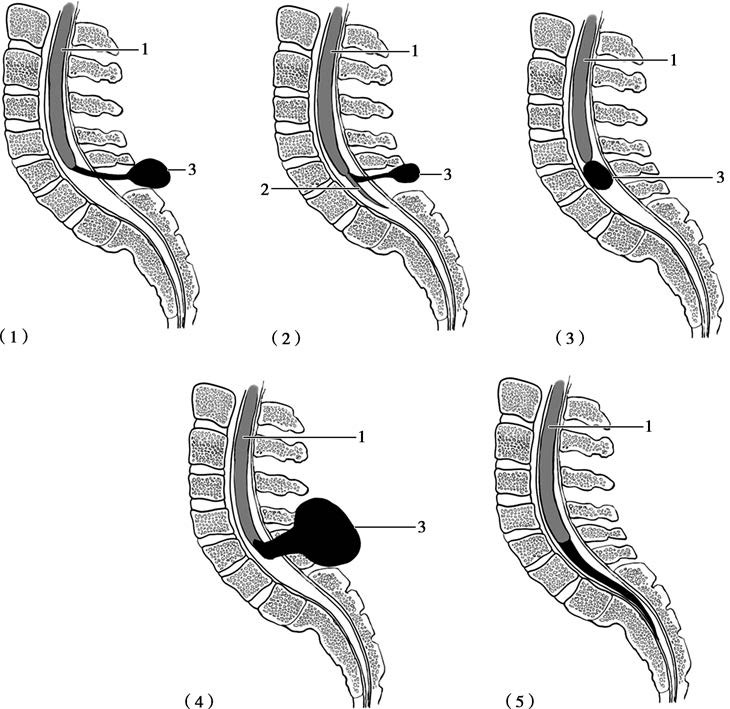
Figure 1 Schematic relationship between the conus medullaris and lipomas in tethered cord syndrome
(1) Lipoma connected to the conus medullaris via fibrous bands.
(2) Lipoma connected to the filum terminale via fibrous bands.
(3) Lipoma directly connected to the conus medullaris.
(4) Lipoma traversing the fascia and connecting to the conus medullaris.
(5) Elongated, thickened filum terminale or transformed lipoma shape.
1, Spinal cord
2, Filum terminale
3, Lipoma
Treatment
Surgery is currently the only effective treatment option. The primary goals of surgical intervention are to release spinal cord tethering and nerve compression, restore local microcirculation, correct associated deformities, and promote recovery of neural function. In cases with concurrent lipomas, the main surgical objective is detethering and volume reduction, aiming to remove the tumor as much as possible while minimizing complications such as spinal cord injury. Earlier surgical intervention generally achieves better outcomes; however, postoperative risks include adhesion recurrence and retethering, which may necessitate reoperation.