The most common form of spina bifida is the absence of the spinous processes and vertebral arches, resulting in dorsal opening of the spinal canal. It most frequently occurs in the lumbosacral region. Overt spina bifida can be classified into the following types:
- Meningocele: Commonly found in the lumbar or lumbosacral region. The meninges, along with cerebrospinal fluid (CSF), form a cystic protrusion under the skin, while the spinal cord and spinal nerves maintain normal position and morphology. Approximately one-third of cases exhibit neurological deficits. This type is the least severe and has a good prognosis.
- Myelomeningocele: The spinal cord and/or spinal nerves protrude along with the meninges through a bony defect, forming a cystic sac that adheres to surrounding structures.
- Myelocele: The spinal cord is exposed, and the spinal cord along with the meninges protrudes outside the spinal canal through the defect in the vertebral arches.
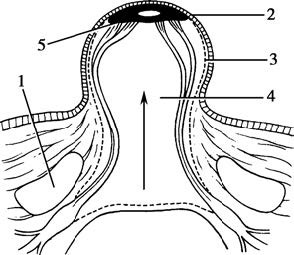
Figure 1 Cross-sectional view of myelomeningocele
1, Vertebral arch
2, Skin
3, Meninges
4, Spinal canal
5, Spinal cord and its dilated central canal
Clinical Manifestations
The clinical manifestations can be categorized into the following three aspects:
Local Manifestations
Skin Abnormalities
Visible signs on the skin, such as shallow dimples, excessive hair growth, capillary hemangioma-like lesions, or sinus tracts, may indicate neural tube closure defects.
Local Masses
A protruding mass near the midline in the lumbosacral region, lower thoracic region, cervical spine, or upper thoracic region is often detectable at birth. About 80% of lesions are located in the lumbosacral region. The size of certain masses may increase during crying or exertion. Masses containing primarily fluid yield positive results in transillumination tests, while masses associated with intraspinal or extraspinal lipomas are more solid in nature.
Neurological Impairment of the Spinal Cord and Nerves
Motor and Sensory Disorders in the Lower Limbs
Signs such as asymmetry in spontaneous movement of neonatal lower limbs, difficulty in dressing due to abnormal muscle strength or tone, and abnormal joint positions (e.g., clubfoot) suggest neurological damage. Motor impairment is primarily characterized by flaccid paralysis. Detailed physical examinations identifying sensory level deficits and affected motor groups can help determine the segment of neural involvement and aid in prognosis assessment.
Sphincter Dysfunction
Features such as reduced voiding frequency, diminished anal sphincter tone, and decreased anal folds, as well as fecal overflow, provide diagnostic insights.
Clinical Symptoms Associated with Congenital Malformations
Conditions such as hydrocephalus, Chiari malformations, scoliosis, or cutaneous sinus tracts may occur concurrently, leading to corresponding clinical symptoms.
Manifestations of Ruptured Cystic Spina Bifida
Cases with rupture of the cystic lesion exhibit exposed contents and leakage of CSF, which are readily apparent clinically.
Diagnosis
In addition to the typical clinical manifestations described above, imaging techniques such as X-ray, three-dimensional computed tomography (3D-CT), and magnetic resonance imaging (MRI) are required to confirm the diagnosis and distinguish it from other conditions. X-ray imaging of the spine serves as an initial diagnostic tool to determine the extent of bony defects. Spinal 3D-CT provides a detailed view of the bony abnormalities, while MRI reveals the specifics of the spinal defect, such as low-lying spinal cord, thickened terminal filum, associated lipomas, and the composition of the protrusion.
Treatment
Non-Surgical Treatment
Spina bifida cases associated with severe hydrocephalus, significant spinal deformities, other congenital organ malformations, paralysis, or cystic spina bifida involving the thoracolumbar spine have a high neonatal mortality rate. For these infants, surgical intervention may be delayed until they are stabilized and have passed the critical life-threatening period.
Surgical Treatment
Surgical intervention is necessary for all cases of overt spina bifida. The optimal timing for surgery is between 1 and 3 months after birth; however, cases with extremely thin cyst walls require earlier intervention. Emergency surgery is required for infants with exposed spinal cord or ruptured myelomeningocele.
The key objectives of surgical treatment include detethering and releasing adhesions, addressing associated lesions, restoring spinal cord coverage, and performing multilayer repair of the dura mater, fascia, and subcutaneous layers, followed by tension-free skin closure. Long-term follow-up is necessary. A multidisciplinary approach is often required for the management of orthopedic issues such as spinal deformities and joint corrections, as well as the treatment of neurogenic bladder.