Cranial encephalocele, also known as cranium bifidum, cystic encephalocele or cystic meningocele, can be classified based on the contents of the protrusion:
- Meningocele: The protrusion consists of meninges and cerebrospinal fluid (CSF).
- Encephalocele: The protrusion consists of meninges and brain parenchyma, without CSF.
- Cystic Meningoencephalocele: The protrusion consists of meninges, brain parenchyma, and part of the ventricles, with CSF present between the brain parenchyma and meninges.
- Cystic Encephalocele: The protrusion consists of meninges, brain parenchyma, and part of the ventricles, but without CSF between the brain parenchyma and meninges.
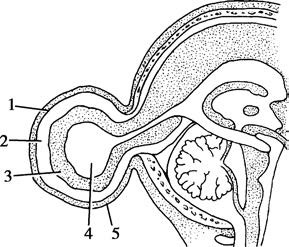
Figure 1 Schematic diagram of cystic meningoencephalocele
1, Meninges
2, Cerebrospinal fluid
3, Brain tissue
4, Part of the ventricle
5, Scalp
Clinical Manifestations and Diagnosis
Cranial encephaloceles most commonly occur along the midline of the skull, with fewer cases appearing off-center. The occipital region accounts for approximately 75% of cases, while the nasion accounts for about 15%. It can also occur in the sphenoid bone, ethmoid bone, or orbits. Encephaloceles in the cranial vault typically manifest as a localized mass, which is apparent at birth and progressively enlarges over time. The texture, translucency, and responsiveness to changes in posture or thoracoabdominal pressure depend on the contents of the protrusion. Palpation may reveal skull defects. In cases involving brain malformations, such as hypoplasia or hydrocephalus, neurological defects such as limb paralysis, contractures, or seizures may be observed.
Cystic encephaloceles at the cranial base often present at the nasion, accompanied by hypertelorism, reduced orbital size, nasal obstruction causing respiratory difficulty, and in some cases, nasolacrimal duct inflammation. Cranial nerve involvement can also lead to corresponding symptoms and signs.
Most cases are diagnosed at birth or within the first month of life by observing cranial morphology. CT and MRI can assist in confirming the diagnosis and differentiating it from other conditions.
Auxiliary Examinations
CT imaging provides detailed information on the location, size, and contents of the encephalocele as well as the presence of associated conditions such as brain hypoplasia or hydrocephalus. MRI offers clearer visualization of brain malformations and the composition of the protrusion. Prenatal detection is also possible through ultrasound imaging, maternal serum, and amniotic fluid alpha-fetoprotein testing, allowing targeted interventions during pregnancy.
Treatment
Surgical intervention is recommended before the age of one if conditions permit. The primary goals of surgery are to close the cranial defect, excise the sac wall, preserve neurological function, reposition protruded brain tissue, and reconstruct the skin, considering both functional and cosmetic outcomes.
For encephaloceles located in the cranial vault, the skull defect does not necessarily require immediate repair; repair of the dura mater and scalp is sufficient. Encephaloceles located at the cranial base often require intracranial surgical repair of both the skull defect and the dura mater. In cases where hydrocephalus is present, addressing the hydrocephalus should take priority. Severe brain malformations or encephaloceles containing brainstem tissue are considered relative contraindications for surgery.