Moyamoya disease (MMD), also known as abnormal vascular networks at the base of the brain, is characterized by stenosis or occlusion of the intracranial segment of the internal carotid artery, leading to the development of pathological vascular networks at the base of the brain. These abnormal networks resemble a "puff of smoke" on cerebral angiography, which is the origin of the disease's name. The prevalence of MMD is higher in Asia compared to North America. The disease has two incidence peaks: in individuals younger than 10 years old and those aged 30–39 years, with a slight predilection for females. Evidence indicates a familial predisposition, though its genetic basis has not yet been conclusively confirmed.
Etiology
The exact cause of MMD remains unclear. Some studies have identified elevated levels of basic fibroblast growth factor in the dura mater and arterial flaps of patients. The internal elastic lamina of affected vessels may show thinning or thickening.
Secondary moyamoya, also referred to as moyamoya syndrome, may occur in association with other conditions such as atherosclerosis, fibromuscular dysplasia, pseudoxanthoma elasticum, cerebral arteritis, post-radiation vasculopathy, or leptospirosis-induced cerebral arteritis. Patients with MMD also show congenital vessel wall defects and a propensity for developing aneurysms, which may result in subarachnoid hemorrhage (SAH) and are often mistakenly attributed to the moyamoya vessels themselves.
Clinical Manifestations
MMD most commonly affects children and young adults and may present as either ischemic or hemorrhagic stroke.
Cerebral Ischemia
Cerebral ischemia is more common in children and may present as recurrent episodes. Symptoms include transient ischemic attacks (TIA) and cerebral infarction. Activities such as straining, heavy exertion, or excessive hyperventilation (e.g., playing wind instruments, crying, or shouting) may trigger neurological symptoms, potentially due to hypocapnia-induced reactive vasoconstriction. Patients may experience alternating hemiparesis in both limbs and/or aphasia, along with cognitive decline. Some individuals report recurrent headaches or seizures.
Cerebral Hemorrhage
Hemorrhagic presentations tend to occur at an older age than ischemic presentations. Rupture of microaneurysms on abnormal vascular networks may cause SAH, intracerebral hemorrhage, or intraventricular hemorrhage, sometimes forming a ventricular cast. Patients often experience an acute onset of symptoms, including sudden headache, vomiting, altered consciousness, and, in some cases, hemiparesis.
Diagnosis
Head CT and MRI
CT and MRI scans may reveal cerebral infarction, brain atrophy, or intraventricular hemorrhage forming a cast. CTA and MRA imaging can demonstrate the characteristic "smoke-like" vascular networks at the base of the brain.
Cerebral DSA
Cerebral digital subtraction angiography (DSA) typically shows stenosis or occlusion of the supraclinoid segment of the internal carotid artery. Thin abnormal vascular networks in the basal ganglia exhibit a "smoke-like" appearance. Extensive vascular collateralization is often seen, including networks between the posterior cerebral artery and the pericallosal artery, as well as connections between the external carotid artery and the temporal artery. Angiography aids not only in diagnosing MMD but also in identifying suitable donor vessels for revascularization surgery and detecting associated aneurysms.
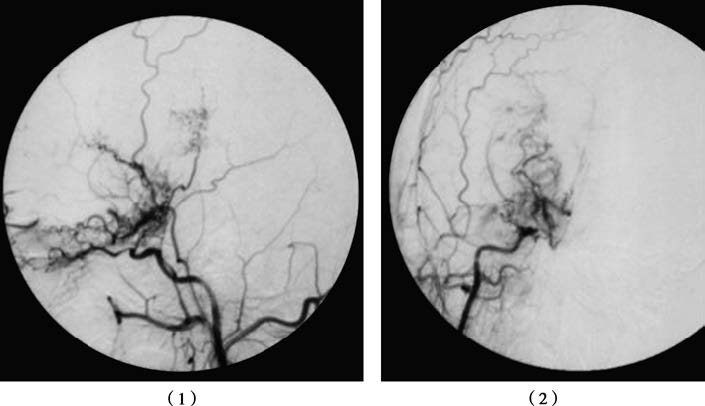
Figure 1 Moyamoya disease
DSA imaging of the right common carotid artery demonstrates occlusion of the right middle cerebral artery with moyamoya-like vascular formation at the terminal segment of the internal carotid artery: (1) lateral view of the right common carotid artery; (2) frontal view of the right common carotid artery.
Treatment
Pharmacological Treatment
Common medical treatments include antiplatelet agents, anticoagulants, calcium channel blockers, corticosteroids, and mannitol.
Surgical Treatment
Cerebral revascularization procedures are effective in reducing the incidence of ischemic strokes and TIAs. These procedures include superficial temporal artery-to-middle cerebral artery (STA-MCA) bypass, encephalomyosynangiosis (EMS), and encephaloduroarteriosynangiosis (EDAS). For patients with acute intracerebral hemorrhages causing brain compression, urgent surgical evacuation of the hematoma may be required. In cases of isolated intraventricular hemorrhage, frontal horn puncture and drainage may be performed. If hydrocephalus develops after hematoma resorption, ventriculoperitoneal shunting can be considered. Vasodilatory treatments may be beneficial for patients with ischemic symptoms.
Secondary Moyamoya Syndrome
Treatment focuses on addressing the underlying cause of the secondary moyamoya syndrome.