Intracranial arteriovenous malformation (AVM) is characterized by a pathological tangle of abnormal blood vessels comprising one or more feeding arteries and draining veins. These vascular malformations may enlarge as the body develops. AVMs can vary in size, with small AVMs measuring less than 1 cm in diameter and large AVMs reaching diameters of up to 10 cm. The brain tissue surrounding the malformed vessels often becomes atrophic due to ischemia and shows gliosis. The arachnoid on the surface of malformed vessels appears thickened and white. Intracranial AVMs can occur in any part of the brain, with those in the cerebral hemispheres typically presenting a wedge shape, with the apex pointing toward the lateral ventricle.
Clinical Manifestations
Hemorrhage
Rupture and bleeding from AVMs often occur within the brain parenchyma but can also lead to intraventricular or subarachnoid hemorrhage. Hemorrhage is the initial symptom in 30%–65% of AVM cases, most commonly occurring between the ages of 20 and 40 years. Symptoms following bleeding include impaired consciousness, headache, and vomiting. AVMs that have a single feeding artery, are small, are deeply located, or are in the posterior cranial fossa are more prone to acute rupture and bleeding. For women, the risk of AVM hemorrhage increases during pregnancy.
Seizures
Seizures are often the first symptom in patients with AVMs located in the frontal or temporal lobes. This is related to ischemia around the lesion, gliosis, and cortical irritation by hemosiderin following hemorrhage. Chronic refractory seizures can lead to hypoxia in brain tissue, potentially resulting in cognitive decline.
Intermittent Localized or General Headache
This symptom may be caused by dilation of feeding arteries, draining veins, or venous sinuses, as well as minor AVM bleeding, hydrocephalus, or increased intracranial pressure.
Neurological Deficits
Due to vascular steal from the AVM, intracranial hemorrhage, or associated hydrocephalus, patients may develop progressive deficits in motor function, sensation, visual fields, or speech. In some cases, symptoms may include intracranial bruits or trigeminal neuralgia.
Aneurysm of the Vein of Galen in Children
AVMs involving the vein of Galen, also referred to as aneurysms of the vein of Galen, may cause heart failure and hydrocephalus in pediatric cases.
Diagnosis
CT Imaging of the Head
Enhanced CT scans often show AVMs as areas of mixed density, with no midline shift in the brain. In the acute phase of hemorrhage, CT imaging is useful to determine the volume and location of the hemorrhage and the presence of hydrocephalus.
MRI of the Head
Due to high blood flow within the lesion, AVMs typically present with a flow void phenomenon on MRI, highlighting the anatomical relationship of the malformed vascular tangle with surrounding brain structures. This information provides guidance for selecting the surgical approach for AVM removal.
Cerebral Angiography
Cerebral angiography provides details on the size, extent, feeding arteries, draining veins, and flow velocity of the AVM.
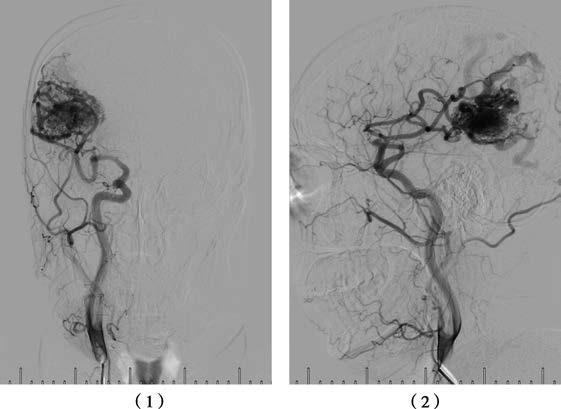
Figure 1 Right common carotid artery DSA
(1) Anteroposterior view showing a right parieto-occipital AVM.
(2) Lateral view showing a right parieto-occipital AVM.
CTA and MRA
These modalities are useful for screening AVM patients or for follow-up evaluations.
Electroencephalography (EEG)
For cerebral hemisphere AVMs, EEG often reveals slow waves or spike waves. Intracranial EEG monitoring during surgery can provide information for the removal of epileptogenic foci, potentially reducing postoperative seizure activity.
Treatment
Surgical Resection
Surgical resection is the preferred method for curing AVMs, as it eliminates the risk of hemorrhage and restores normal cerebral blood flow. During surgery or postoperatively, large AVM resections can sometimes lead to acute brain swelling or hemorrhage, a phenomenon referred to as normal perfusion pressure breakthrough (NPPB), which poses significant risks. Current approaches often involve hybrid procedures, such as intraoperative embolization followed by surgical resection of large AVMs. Laser Doppler flowmetry is used intraoperatively to monitor local cortical blood flow changes around the AVM before and after resection. Studies have shown that cortical blood flow around the lesion increases after AVM resection and may persist for 24–48 hours. Maintaining low blood pressure levels during this period is one approach to reducing the risks associated with NPPB.
Non-Surgical Cases
AVMs located in deep and critical functional brain regions, such as the brainstem or diencephalon, are less suitable for surgical resection.
Post-Treatment Follow-Up
Cerebral angiography is performed after treatment to verify whether the abnormal vascular structures have been completely obliterated. Residual vascular malformations may require additional treatments to prevent rebleeding. For AVMs with a diameter of less than 3 cm or for residual AVMs following surgery, endovascular treatment or stereotactic radiosurgery (e.g., Gamma Knife) may be considered, though there remains a risk of hemorrhage during the treatment period.