Subarachnoid hemorrhage (SAH) refers to bleeding caused by the sudden rupture of intracranial or intraspinal blood vessels, leading to blood accumulation in the subarachnoid space. SAH can be classified into spontaneous and traumatic forms, with this discussion focusing solely on spontaneous SAH.
Etiology
Intracranial aneurysms and vascular malformations of the brain or spinal cord account for about 70% of spontaneous SAH cases, with aneurysms being more common than malformations. Other causes include atherosclerosis, moyamoya disease, stroke caused by brain tumors, hematologic disorders, arteritis, encephalitis, meningitis, and complications of anticoagulation therapy.
Clinical Manifestations
Severe Headache
In most cases, triggering factors such as emotional stress, constipation, or coughing precede aneurysm rupture. Patients experience sudden headaches described as "explosive," accompanied by nausea, vomiting, pallor, cold sweats, dizziness, neck or back pain, or lower limb discomfort. Meningeal irritation signs tend to develop within 1–2 days of the hemorrhage. If an aneurysm rupture is not promptly treated, rebleeding may occur within 1–2 weeks, with approximately one-third of cases resulting in death due to rebleeding.
Transient Loss of Consciousness
About half of patients experience transient episodes of impaired consciousness, while severe cases may progress to coma.
Seizures
Around 20% of patients experience seizures following the hemorrhage.
Cranial Nerve Damage
Aneurysms located at the internal carotid artery-posterior communicating artery junction, the apex of the basilar artery, or the posterior cerebral artery may lead to ipsilateral oculomotor nerve palsy.
Visual Impairment
Subarachnoid hemorrhage extending along the optic nerve sheath can cause retinal hemorrhage, as observed during fundoscopic examination. Extensive bleeding may involve the vitreous body, leading to visual impairment. Large aneurysms pressing on the optic nerve or optic radiation may result in bitemporal hemianopia or homonymous hemianopia.
Intracranial Murmurs
Approximately 1% of patients with intracranial arteriovenous malformations or aneurysms may present with audible intracranial murmurs. Low-grade fever may develop several days after the onset of SAH in some cases.
Retinal or Vitreous Hemorrhage (Terson Syndrome)
The presence of retinal or vitreous hemorrhage has been associated with a high mortality rate.
Differential diagnosis of spontaneous SAH is summarized in Table 1. To assess disease severity, select imaging or surgical timing, and evaluate treatment outcomes, the Hunt-Hess grading system is often employed.

Table 1 Differential diagnosis of spontaneous subarachnoid hemorrhage (SAH)
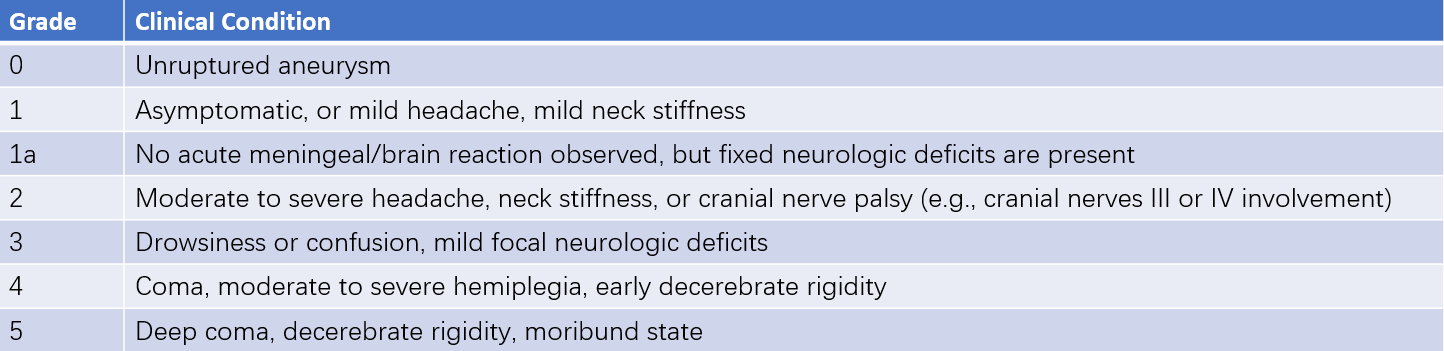
Table 2 Hunt-Hess grading system for subarachnoid hemorrhage
Note: For patients with severe systemic comorbidities (e.g., hypertension, diabetes, severe atherosclerosis, chronic obstructive pulmonary disease) or severe vasospasm detected on angiography, an additional grade is added.
Diagnosis
Head CT
Non-enhanced high-resolution CT performed within 48 hours of SAH onset can detect SAH in over 95% of cases. CT images are most sensitive within the first week, showing elevated densities in the cerebral sulci and cisterns. Certain bleeding patterns can help identify the likely location of aneurysm rupture, such as blood pooling in the perimesencephalic cistern for internal carotid aneurysm rupture, blood in the Sylvian fissure for middle cerebral artery aneurysms, blood in the interhemispheric cistern for anterior cerebral artery aneurysms, and blood in the interpeduncular or perimesencephalic cisterns for basilar artery aneurysms. CT angiography (CTA) is a preferred non-invasive test for diagnosing aneurysms and vascular malformations and aids in the differential diagnosis of SAH.
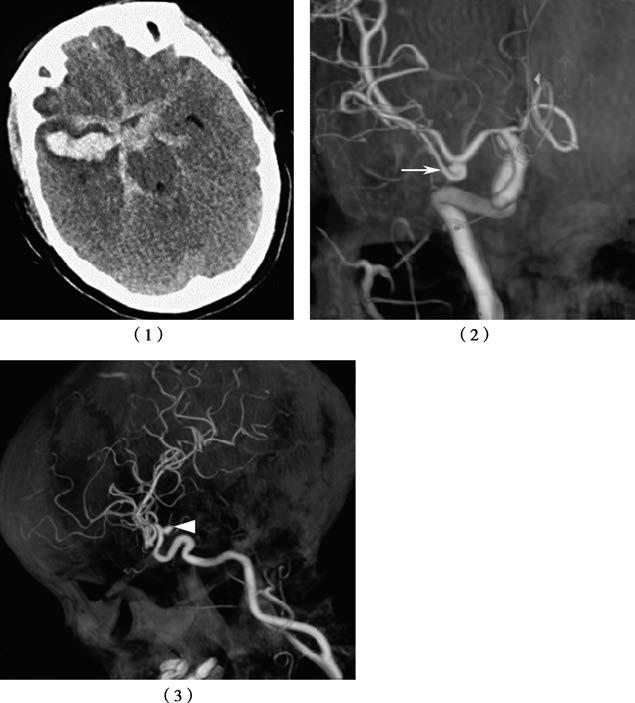
Figure 1 Multiple aneurysms with subarachnoid hemorrhage
1, CT shows subarachnoid hemorrhage, with severe involvement in the right Sylvian fissure.
2, The right middle cerebral artery aneurysm is identified as the culprit aneurysm causing the hemorrhage.
3, The right internal carotid artery aneurysm is also observed.
Head MRI
MRI is less sensitive than CT during the first 24–48 hours after SAH (due to insufficient deoxyhemoglobin) but becomes more sensitive during the subacute phase (4–7 days, peaking at 10–20 days). Magnetic resonance angiography (MRA) has poor sensitivity for aneurysms smaller than 3 mm but is often used for screening in high-risk patients.
Digital Subtraction Angiography (DSA)
DSA provides detailed information on the size, location, and number of aneurysms; presence of vascular spasms; and arterial supply and venous drainage of arteriovenous malformations. It also helps evaluate collateral circulation and establish the cause of SAH. Spinal angiography is recommended in patients suspected of having spinal arteriovenous malformations.
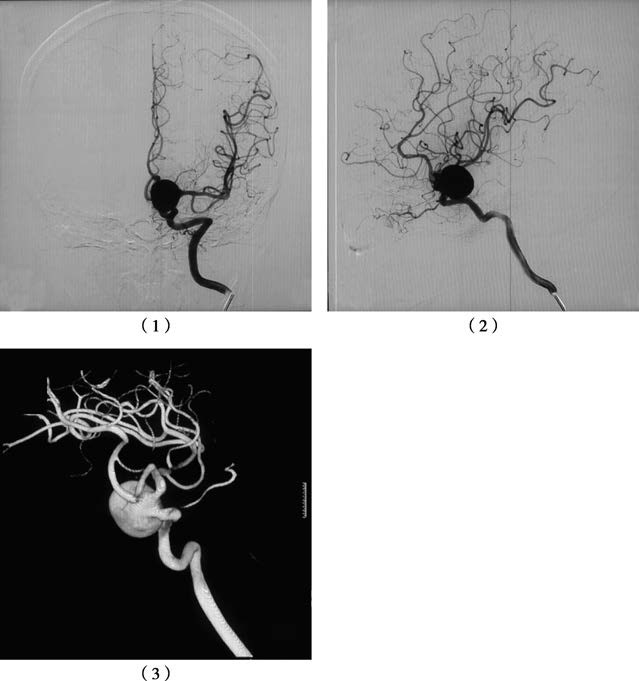
Figure 2 Giant aneurysm of the left internal carotid artery-posterior communicating segment on DSA
1, Anteroposterior view of the left internal carotid artery.
2, Lateral view of the left internal carotid artery.
3, Three-dimensional angiography for detailed visualization.
Lumbar Puncture
In cases of confirmed SAH, lumbar puncture is not routinely required. When intracranial pressure is elevated in SAH, performing a lumbar puncture to collect cerebrospinal fluid may risk precipitating brain herniation.
Treatment
Acute Phase Management
During the acute phase of hemorrhage, strict bed rest is necessary. Hemostatic agents may be used. Severe headache can be managed with analgesics and sedatives, and bowel movements should remain regular. Elevated intracranial pressure may be treated with dehydration therapy using a 20% mannitol solution.
Etiological Treatment
Early treatment targeting the underlying cause is preferred. This includes microsurgical clipping or endovascular coiling for aneurysm repair, as well as surgical removal of arteriovenous malformations or brain tumors as indicated.