Craniocerebral missile injury is common during wartime but also occurs in civilian settings. Its incidence is second only to extremity injuries, yet it has the highest mortality rate.
Classification
Craniocerebral missile injuries can be classified into the following simplified categories:
- Scalp Soft Tissue Injury: Involves scalp damage with an intact skull; a minority of patients may have localized cerebral contusions.
- Non-Penetrating Injury: Includes scalp injury, skull fracture, and intact dura mater, but with cerebral contusions, lacerations, or even intracranial hematoma formation.
- Penetrating Injury: Characterized by scalp injury, skull fracture, and dural rupture, with severe brain damage often accompanied by intracranial hematoma. These injuries are further categorized by mechanism:
- Blind Tract Injury: The projectile enters through the cerebral convexity or facial region and remains in the cranial cavity. Bone fragments and debris typically accumulate near the entry site, while the projectile lodges at the distal end of the tract. In rare cases, the projectile rebounds after striking the contralateral inner skull table, causing a "ricochet injury" with severe brain damage.
- Through-and-Through Injury: The projectile passes completely through the skull, creating entry and exit wounds. The entry site contains bone fragments, while the exit site has a larger bone defect. These injuries often involve critical brain structures or ventricles due to the long tract.
- Tangential Injury: The projectile grazes the skull and brain without lodging inside. A groove-like defect forms in the skull and brain, with bone fragments scattered in superficial brain tissue.
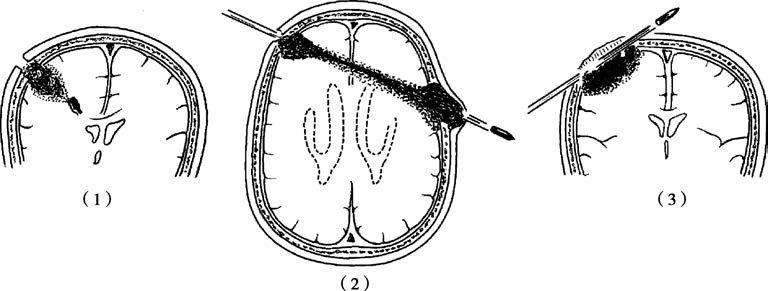
Figure 1 Craniocerebral penetrating injuries
(1) Blind tract injury, (2) Through-and-through injury, (3) Tangential injury
Mechanisms and Pathology
The severity of firearm craniocerebral injuries depends on the projectile’s shape, velocity, and size. High-velocity bullets (e.g., modern firearms) are streamlined and penetrate easily, often causing through-and-through injuries. Irregular fragments (e.g., shrapnel) have lower penetration and tend to cause blind tract injuries. Brain damage from projectiles is categorized as:
- Tract Injury: The projectile creates a tract of varying length. The extent of damage depends on the projectile’s properties. The tract comprises three layers:
- Destruction Zone: Central area with necrotic, liquefied brain tissue and blood clots, sometimes extruding from the wound.
- Contusion Zone: Surrounding area with petechial hemorrhages and edema, often irreversible.
- Concussion Zone: Outermost layer with no macroscopic changes, typically recovering within days.
- Expansile Injury: High-velocity projectiles cause transient cavitation, leading to diffuse brain damage. Severe cases involve brainstem injury, often resulting in rapid death.
Clinical Manifestations
Consciousness Impairment
Low-velocity injuries (e.g., shrapnel) cause localized damage and rarely induce immediate unconsciousness. High-velocity injuries (e.g., bullets) frequently trigger diffuse brain injury with immediate loss of consciousness. Progressive deterioration of consciousness suggests intracranial hematoma.
Vital Sign Changes
Severe injuries often disrupt vital signs. Brainstem involvement rapidly causes central respiratory/circulatory failure. Signs of elevated intracranial pressure (e.g., slow respiration, bradycardia, hypertension) indicate hematoma or cerebral edema.
Pupillary Changes
Unilateral pupillary dilation and loss of light reflex suggest uncal herniation due to hematoma. Bilateral fixed dilation indicates severe brainstem injury and a terminal state.
Neurological Deficits
Immediate limb paralysis reflects direct damage to motor cortex or pathways. Worsening paralysis often signals hematoma formation within the tract.
Diagnosis
The examination and diagnosis of craniocerebral missile injuries are similar to other types of head injuries, with a particular emphasis on evaluating head and facial wounds as well as associated injuries.
CT scans are routinely performed in patients with craniocerebral missile injuries to determine the injury tract, the location and extent of brain contusion and laceration, the presence of skull fractures, the type, number, size, and location of foreign bodies, and the presence of intracranial hematomas or brain abscesses. If metallic foreign bodies are retained intracranially, head MRI scans are contraindicated.
Treatment
Emergency Treatment
Craniocerebral missile injuries are characterized by sudden onset, severe condition, and rapid progression, requiring intensive efforts to save the patient's life. In cases of critical conditions, emergency treatment is implemented at the site of injury, during transport, or upon arrival at the emergency department, including:
- Wound dressing to reduce bleeding while protecting protruding brain tissue if present.
- Positioning unconscious patients in a lateral or prone position to facilitate the clearance of blood, vomit, or secretions from the mouth, nose, and trachea. Endotracheal intubation may be performed if necessary to ensure airway patency.
- For patients in shock, anti-shock treatment is provided while promptly identifying its causes, such as excessive blood loss from head wounds, thoracic or abdominal organ injuries, or fractures, followed by appropriate management.
Early Debridement
The goal is to convert an open brain injury, contaminated with bleeding, contused brain tissue, and foreign bodies, into a clean, non-actively bleeding, and foreign-body-free closed injury. Early debridement is generally performed within a few hours to 24 hours after the injury. The surgical approach to debridement is similar to that for non-firearm open injuries.
Other Treatments
Treatment is similar to that for closed craniocerebral injuries.