Subdural hematoma (SDH) accounts for approximately 40% of traumatic intracranial hematomas and is often classified as acute or subacute. Chronic subdural hematoma has unique characteristics and is also discussed in this section.
Mechanism of Occurrence
Acute and subacute subdural hematomas primarily result from ruptures of cortical blood vessels. Bleeding at regions such as the frontal pole, temporal pole, and frontotemporal base is often caused by contrecoup cerebral contusions and lacerations. Hematomas resulting from tearing of bridging veins that drain into the venous sinuses or the venous sinuses themselves typically cover a larger area and may occur without associated brain contusions.
The source and mechanism of bleeding in chronic subdural hematomas are not fully understood. These hematomas are more common in elderly individuals, the vast majority of whom have a history of minor head trauma. In a small number of cases without trauma, potential contributing factors may include long-term anticoagulant use, malnutrition, vitamin C deficiency, and vascular disorders. Chronic subdural hematomas often feature membranes of varying thickness.
Clinical Manifestations
Acute and subacute subdural hematomas primarily present with the following:
Consciousness Impairment
Patients with SDH and associated cerebral contusions are often in sustained or progressively worsening coma. Subacute hematomas frequently exhibit a lucid interval.
Increased Intracranial Pressure
Secondary brain edema following injury results in increased intracranial pressure, leading to symptoms such as headache, nausea, vomiting, and alterations in vital signs.
Pupillary Changes
Rapid disease progression due to brain contusions and edema is likely to cause brain herniation, leading to pupillary changes. Early signs include dilated pupils on the side of the hematoma. Without timely intervention, bilateral pupil dilation may occur following herniation, posing a life-threatening risk.
Neurological Signs
Immediate post-trauma neurological deficits, such as hemiplegia, result from cerebral contusion. Gradually developing neurological signs are indicative of brain function area compression by the hematoma or of brain herniation.
Chronic subdural hematomas progress slowly over a prolonged course, often lasting about one month, though they can persist for several months. Clinical manifestations vary widely and are generally divided into three types:
- Symptoms dominated by intellectual and psychological changes, such as dizziness, tinnitus, memory loss, sluggish reactions, or mental disorders.
- Symptoms focused on focal neurological deficits, such as hemiplegia, aphasia, or focal epilepsy.
- Symptoms of increased intracranial pressure, which are rare and often lack clear neurological localization.
The first type is easily misdiagnosed as Alzheimer's disease or a psychiatric disorder, while the latter two types may be confused with intracranial tumors.
Diagnosis
A history of head trauma followed by immediate or progressively worsening consciousness impairment, or a lucid interval accompanied by symptoms of increased intracranial pressure, often suggests acute or subacute subdural hematoma. CT imaging confirms the diagnosis; acute or subacute subdural hematomas appear as crescent-shaped hyperdense, mixed-density, or isodense lesions between the brain surface and the skull, often accompanied by brain contusions and cerebral compression.
Chronic subdural hematomas are prone to misdiagnosis or missed diagnosis. Elderly individuals presenting with symptoms of chronic intracranial pressure increase, intellectual and psychological abnormalities, or neurological dysfunction, especially with a recent history of minor head trauma, should be evaluated for the possibility of chronic subdural hematoma. Timely CT or MRI can confirm the diagnosis. CT imaging reveals crescent-shaped or semilunar hypodense or isodense lesions over the brain surface. MRI shows crescent-shaped or semilunar lesions with low T1 and high T2 signal intensities.
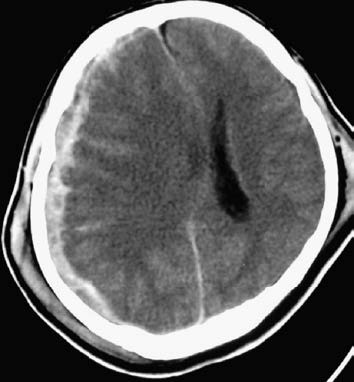
Figure 1 Acute subdural hematoma (CT, right frontoparietal lobe)
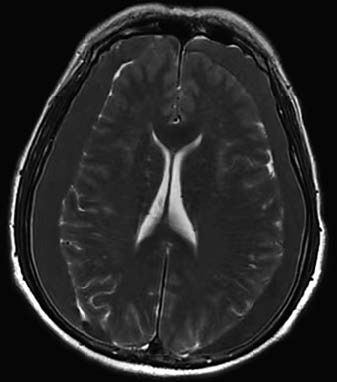
Figure 2 Chronic subdural hematoma (MRI, bilateral frontoparietal lobes)
Treatment
The treatment principles for acute and subacute subdural hematomas are similar to those for epidural hematomas. Subdural hematomas can appear at the site of impact or at contrecoup regions. In critical situations where the hematoma location cannot be confirmed with preoperative CT imaging and craniotomy is urgently required to save the patient's life, burr holes should be created at both the site of impact and the contrecoup site, especially in areas most commonly affected by subdural hematoma such as the frontal pole, temporal pole, and their respective bases. Additionally, as these hematomas are often accompanied by cerebral contusions, postoperative management should address these associated injuries.
For chronic subdural hematoma, patients with significant symptoms often require surgical intervention. Burr hole and catheter drainage is the preferred option. For smaller hematomas, a single burr hole at the parietal eminence is sufficient, whereas larger hematomas may require an additional burr hole in the frontal region. The dura and the hematoma's parietal wall membrane are incised to insert a catheter into the hematoma cavity. As recurrence is possible, follow-up CT or MRI imaging is necessary.