Epidural hematoma (EDH) accounts for approximately 30% of traumatic intracranial hematomas. It is mostly of the acute type and can occur at any age.
Mechanism of Occurrence
The primary sources of epidural hematoma are rupture of the middle meningeal artery, venous sinuses, or bleeding from skull fractures. The middle meningeal artery enters the skull via the foramen spinosum at the base of the middle cranial fossa and travels along the meningeal grooves of the temporal bone. At the pterion, the artery divides into anterior and posterior branches. Both the main trunk and its branches can rupture due to temporal bone fractures, forming a hematoma in the epidural space at the frontotemporal region. Damage to the intracranial venous sinuses (e.g., superior sagittal sinus, transverse sinus), middle meningeal veins, diploic veins, or emissary veins can also result in epidural hematoma. In rare cases, patients without fractures can develop EDH due to the separation of the dura mater from the skull and tearing of small blood vessels on the dura's surface following head trauma.
Epidural hematoma most commonly occurs in the temporal, frontoparietal, and temporoparietal regions. Hematomas caused by rupture of the middle meningeal artery are typically located in the frontotemporal region, with potential extension toward the frontal or parietal regions. Hematomas from anterior branch bleeding are usually found in the frontotemporal area, whereas those from posterior branch bleeding often occur in the temporoparietal region. Hematomas caused by superior sagittal sinus rupture are distributed on one or both sides of the cerebral hemispheres, while those resulting from transverse sinus rupture are typically located in the posterior cranial fossa or saddle both the posterior fossa and occipital region.
Clinical Manifestations
Consciousness Impairment
Progressive impairment of consciousness is the most severe symptom of epidural hematoma. Its progression is closely related to the severity of primary brain injury and the rate of hematoma formation. Clinically, three scenarios are commonly observed:
- Primary brain injury is mild, with no initial loss of consciousness following the injury. Loss of consciousness develops only after the formation of the intracranial hematoma (lucid period → coma).
- Primary brain injury is moderate, with patients initially experiencing a period of unconsciousness, followed by full recovery or improvement, but later lapsing back into unconsciousness (coma → lucid interval or improvement → coma).
- Primary brain injury is severe, with progressive worsening or sustained coma from the outset.
Since primary brain injuries in epidural hematoma are generally mild, scenarios (1) and (2) are more common.
Increased Intracranial Pressure
Symptoms of increased intracranial pressure, such as headache, nausea, and vomiting, are often present during periods of lucid consciousness or improvement before coma. These symptoms may be accompanied by changes in vital signs, including elevated blood pressure and slowed respiration and pulse rates.
Pupillary Changes
When intracranial pressure from an epidural hematoma reaches a critical level, it can result in brain herniation. For supratentorial hematomas, transtentorial herniation often occurs first, leading to worsening consciousness and pupillary changes. Early symptoms include transient pupil constriction on the affected side due to irritation of the oculomotor nerve, which is often brief and may go unnoticed. This is followed by pupil dilation on the affected side due to oculomotor nerve compression. In cases of advanced brain herniation with severe brainstem compression and damage to the oculomotor nucleus in the midbrain, bilateral pupil dilation may develop. Infratentorial hematomas lead to delayed pupillary changes but cause early respiratory dysfunction or arrest.
Neurological Signs
Focal neurological deficits occurring immediately after the injury reflect primary brain damage. Simple epidural hematomas that do not compress functional brain regions exhibit few early neurological signs. However, as the hematoma enlarges and causes transtentorial herniation, contralateral pyramidal tract signs may appear. Advanced brain herniation and brainstem compression can result in decerebrate rigidity.
Diagnosis
The diagnosis of epidural hematoma is based on a history of head trauma combined with a clinical course characterized by immediate post-injury consciousness, followed by coma or a period of lucid consciousness with subsequent impairment. CT imaging typically reveals a fracture line involving the middle meningeal artery or venous sinus grooves, which supports an early diagnosis.
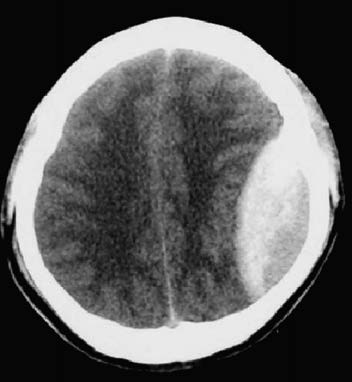
Figure 1 Epidural hematoma (CT, left parietal lobe)
CT scans not only provide direct visualization of the epidural hematoma, which appears as a biconvex or lentiform hyperdense lesion between the inner table of the skull and the dura, but also assess the degree of ventricular compression, midline shift, and coexisting cerebral contusions or edema. Early CT assessment and repeated scans as needed are essential after the injury.
Treatment
Surgical Treatment
Surgical indications include significant symptoms and signs of elevated intracranial pressure, CT evidence of substantial intracranial hematoma causing brain tissue compression, and specific hematoma volumes: supratentorial hematoma >30 mL, temporal hematoma >20 mL, infratentorial hematoma >10 mL, or hematomas causing intracranial pressure elevation from large venous sinus compression. Based on CT findings, hematoma evacuation is performed through craniotomy with bone flap or burr hole approaches, with appropriate hemostasis.
If high dural tension or suspected subdural hematoma persists after hematoma removal, the dura should be opened for further exploration. For critically ill patients who have not undergone timely CT scans, exploratory burr holes should be placed at the fracture site on the side of pupil dilation, followed by bone window expansion and removal of the hematoma.
Non-Surgical Treatment
For stable patients without significant impairment of consciousness, and with CT evidence indicating supratentorial hematoma volumes <30 mL, infratentorial hematoma volumes <10 mL, and midline shift <1.0 cm, non-surgical treatment may be employed under close monitoring of the patient’s condition.