Anatomical Basis
The cranial cavity is divided by the tentorium cerebelli into two compartments: the supratentorial compartment and the infratentorial compartment. The infratentorial compartment accommodates the brainstem and cerebellum. The supratentorial compartment is further subdivided into left and right hemispheres by the falx cerebri, which allows communication between the two hemispheres through the subfalcine foramen under the falx. This anatomical configuration provides greater mobility for both cerebral hemispheres.
The midbrain passes through the tentorial notch and is adjacent to the uncus and hippocampal gyrus of the temporal lobe. The oculomotor nerve, originating from the medial cerebral peduncle, crosses the tentorial notch and travels along the lateral wall of the cavernous sinus to the superior orbital fissure. The opening that connects the cranial cavity to the spinal canal is known as the foramen magnum, where the lower medulla transitions into the spinal cord. The cerebellar tonsils, located on either side of the lower cerebellar vermis, lie along the dorsal surface of the medulla, with their lower margins positioned against the posterior edge of the foramen magnum.
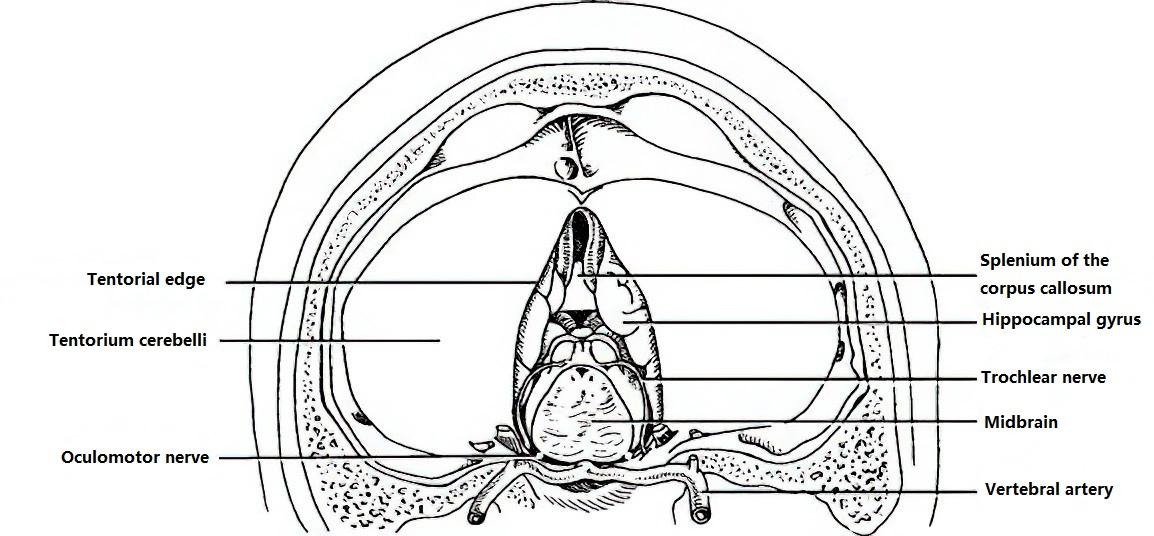
Figure 1 Local anatomical relationships at the tentorial notch (as observed from a supratentorial perspective looking upward).

Figure 2 Local anatomical relationships at the foramen magnum (as observed from an external cranial perspective inward, with dura mater and the atlantoaxial complex removed).
Under conditions of a pressure gradient, brain tissue may be pushed into natural anatomical spaces or pathological openings, such as the tentorial notch, foramen magnum, or subfalcine space. This displacement can compress critical structures, including brain tissue, blood vessels, and cranial nerves, leading to a series of clinical syndromes collectively referred to as brain herniation.
Etiology and Classification
Common causes of brain herniation include the following:
- Various intracranial hematomas, such as epidural, subdural, and intracerebral hematomas.
- Large-area cerebral infarction.
- Intracranial tumors.
- Intracranial abscesses, parasitic infections, and granulomatous lesions.
- Iatrogenic factors, such as performing a lumbar puncture in patients with elevated intracranial pressure, which can exacerbate pressure differences between the cranial cavity and spinal subarachnoid space, triggering herniation.
Brain herniation can be classified based on the displaced brain tissue or the dural aperture through which it passes. Common types include:
- Uncal herniation or transtentorial herniation: The uncus and hippocampal gyrus of the temporal lobe are displaced downward through the tentorial notch.
- Tonsillar herniation or foramen magnum herniation: The cerebellar tonsils and medulla are displaced downward through the foramen magnum into the spinal canal.
- Cingulate herniation or subfalcine herniation: The cingulate gyrus of one hemisphere is displaced across the midline under the falx cerebri to the opposite side.
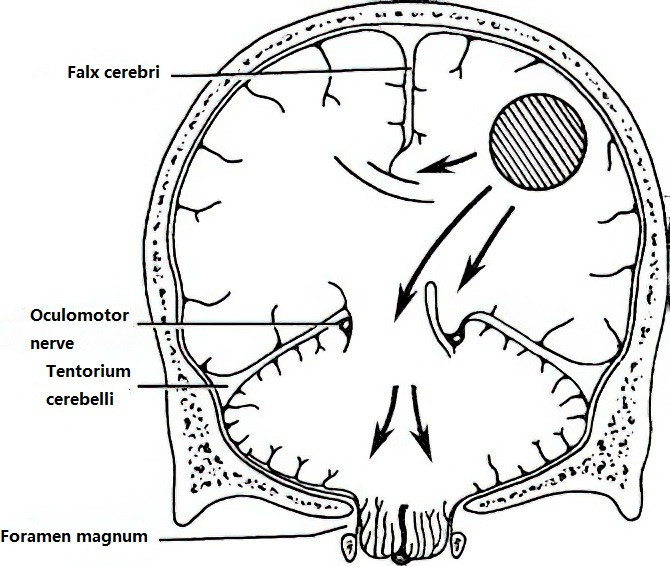
Figure 3 Schematic representation of subfalcine herniation (top), transtentorial herniation (middle), and foramen magnum herniation (bottom).
Pathophysiology
In transtentorial herniation, brain tissue moves beneath the tentorium cerebelli, compressing and displacing the brainstem. Ipsilateral cerebral peduncle compression can result in contralateral hemiparesis, while ipsilateral oculomotor nerve compression may cause initial nerve irritation and subsequent paralysis. The displaced uncus and hippocampus may compress the posterior cerebral artery against the edge of the tentorial notch, leading to ischemic necrosis in the occipital cortex.
In foramen magnum herniation, the medulla is directly compressed, resulting in rapid respiratory arrest. Brain herniation further obstructs cerebrospinal fluid circulation, worsening intracranial pressure and creating a vicious cycle that rapidly deteriorates the patient's condition.
Clinical Manifestations
The clinical features vary depending on the type of brain herniation. The primary characteristics of transtentorial herniation and foramen magnum herniation are summarized as follows:
Transtentorial Herniation
Symptoms of Elevated Intracranial Pressure
Severe headache, frequent vomiting unrelated to eating, and progressively worsening headaches are accompanied by agitation. Acute herniation may occur without visible papilledema.
Pupillary Changes
Initially, irritation of the ipsilateral oculomotor nerve may result in a contracted pupil with sluggish light reflex. As the condition progresses, nerve paralysis leads to gradual pupil dilation with the loss of both direct and consensual light reflexes, ptosis of the ipsilateral eyelid, and outward deviation of the affected eye. If the herniation progresses further, bilateral pupil dilation with loss of light reflexes may occur due to damage to the midbrain oculomotor nuclei and is often a sign of an impending fatal outcome.
Motor Impairments
Weakness or paralysis in the contralateral limb is present, with positive pathological reflexes. Severe cases may exhibit decerebrate rigidity, signaling significant brainstem damage.
Consciousness Alterations
Changes in consciousness, ranging from drowsiness to deep coma, occur due to the involvement of the ascending reticular activating system in the brainstem.
Disruption of Vital Signs
Dysfunction or failure of brainstem life centers may cause a slowing or irregularity in heart rate, fluctuating blood pressure, irregular breathing patterns, profuse sweating or anhidrosis, and facial redness or pallor. Hyperpyrexia exceeding 41°C or an inability to maintain body temperature may also occur. The patient ultimately succumbs to respiratory and circulatory failure, characterized by respiratory arrest, hemodynamic collapse, and cardiac arrest.
Foramen Magnum Herniation
In cases of rapid intracranial pressure elevation, patients may exhibit severe headache, frequent vomiting, neck stiffness, and forced head positioning. Vital sign disruption appears early, whereas altered consciousness develops later. Bilateral pupil size may fluctuate due to hypoxia in the brainstem. Severe damage to the respiratory centers within the medulla often results in sudden respiratory arrest and early death.
Treatment
Brain herniation is caused by a rapid increase in intracranial pressure. Once diagnosed, intravenous administration of hyperosmolar agents to reduce intracranial pressure is typically required to alleviate the condition and create a window of time for further intervention. For cases with a clear etiology, addressing the underlying cause as soon as possible is critical—for example, removing an intracranial hematoma or resecting a brain tumor. When the diagnosis is uncertain or the cause cannot be resolved, certain surgical procedures may be performed to lower intracranial pressure and manage brain herniation.
External Ventricular Drainage
Rapid drilling or trepanation of the frontal or occipital region enables puncture of the lateral ventricle for the placement of a drainage catheter. This method facilitates cerebrospinal fluid (CSF) drainage, effectively reducing intracranial pressure rapidly.
Cerebrospinal Fluid Shunting
In cases of hydrocephalus, procedures such as ventriculoperitoneal shunt (V-P shunt), lumbar cistern-to-peritoneal shunt, or lateral ventricle-to-atrium shunt can be employed. For aqueductal obstruction or stenosis, neuroendoscopic third ventriculostomy (ETV) may be considered.
Decompression Surgery
For transtentorial herniation, decompression can be achieved through temporalis muscle decompression.
In cases of foramen magnum herniation, occipital decompression is an option.
For large-area cerebral infarction or severe brain edema caused by traumatic brain injury, which results in elevated intracranial pressure, decompressive craniectomy can be performed. These approaches are collectively referred to as external decompression techniques.
During craniotomy, if brain tissue swelling is observed, and intracranial hematoma has been ruled out, removal of nonviable tissue or partial resection of nonfunctional brain regions may be conducted as an internal decompression strategy to alleviate pressure.