Increased intracranial pressure (ICP) is a common clinical syndrome in neurosurgery. Various pathological conditions, such as craniocerebral trauma, tumors, vascular diseases, hydrocephalus, and inflammation, may reach a stage where intracranial pressure exceeds its normal upper limit, leading to this syndrome. Understanding the material basis of intracranial pressure, becoming familiar with its regulatory mechanisms, and mastering the pathogenesis and common treatment strategies for increased intracranial pressure are key components in the study of neurosurgery.
Formation and Normal Values of Intracranial Pressure
The material basis of intracranial pressure includes brain tissue, cerebrospinal fluid (CSF), and blood circulating within the cerebral vasculature. Once the cranial sutures are closed, the intracranial volume becomes fixed, which is approximately 1,400–1,500 ml in normal adults. These three components occupy specific volumes within the cranial cavity, maintaining a steady pressure known as intracranial pressure (ICP). In adults, normal ICP (in the lateral decubitus position) ranges from 70–200 mmH2O, while in children, it ranges from 50–100 mmH2O.
Regulation and Compensation of Intracranial Pressure
Under physiological conditions, blood pressure and respiration cause minor fluctuations in intracranial pressure. When ICP increases, the three components within the cranial cavity contribute differently to its regulation. Brain tissue is minimally compressible over short periods, so ICP adjustments primarily rely on regulating cerebral blood flow as well as the distribution and secretion of CSF. When ICP increases, CSF secretion decreases while its absorption increases, compensating for the heightened pressure. When ICP decreases, CSF secretion increases while absorption decreases, helping maintain normal ICP. CSF accounts for about 10% of the total intracranial volume, while blood volume fluctuates between 2% and 11%, depending on cerebral blood flow. An increase of more than 5% in intracranial contents or a reduction of 8%–10% in intracranial capacity may lead to increased ICP.
Etiology
The causes can be classified into five major categories:
- Intracranial space-occupying lesions that encroach on cranial space, such as intracranial hematomas, tumors, or brain abscesses.
- Enlargement of brain tissue volume, such as in cases of cerebral edema.
- Impaired circulation and/or absorption of CSF, leading to high-pressure hydrocephalus.
- Cerebral hyperperfusion or obstructed venous outflow, as seen in cases of brain swelling or venous sinus thrombosis.
- Congenital abnormalities that reduce cranial volume, such as craniosynostosis or basilar invagination.
Pathophysiology
Factors Influencing Increased Intracranial Pressure
Age
In infants with unclosed cranial sutures, increased ICP can widen the sutures, enlarging the intracranial volume. In elderly individuals, brain atrophy increases compensatory intracranial space.
Rate of Lesion Expansion
The relationship between the increase in intracranial lesion volume and the rise in ICP follows an exponential curve known as the volume-pressure curve. Early in the disease course, slow lesion growth causes only minor changes in ICP. However, when compensatory mechanisms are overwhelmed, the condition may rapidly deteriorate, leading to an acute ICP crisis or brain herniation within a short time.
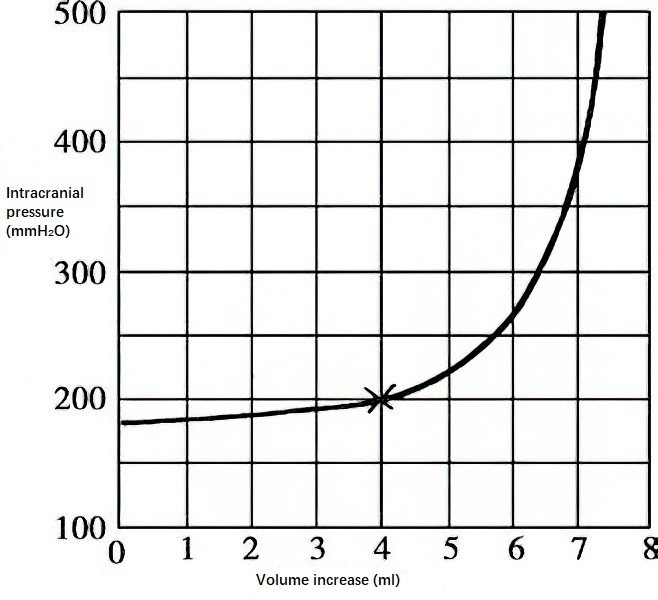
Figure 1 Intracranial volume-pressure relationship curve
Location of the Lesion
Space-occupying lesions in the midline of the brain or posterior fossa are more likely to cause obstructive hydrocephalus, causing pronounced and rapidly progressive symptoms of increased ICP. Venous sinus involvement may impair venous outflow or CSF absorption, resulting in early symptoms of increased ICP.
Degree of Associated Cerebral Edema
Conditions such as metastatic brain tumors, radiation therapy for brain tumors, and inflammatory responses often involve significant cerebral edema, leading to early onset of increased ICP symptoms.
Systemic Conditions
Systemic disorders, such as electrolyte and acid-base imbalances, uremia, hepatic encephalopathy, toxemia, and infections, may cause secondary cerebral edema, contributing to increased ICP. High fever and hypoxia can further exacerbate the severity of increased ICP.
Consequences of Increased Intracranial Pressure
Increased intracranial pressure (ICP) can result in a series of central nervous system functional disruptions and pathological changes.
Reduced Cerebral Blood Flow, Leading to Cerebral Ischemia or Even Brain Death
In normal adults, approximately 1,200 ml of blood enters the cranial cavity per minute, and this is regulated by the brain's autoregulatory mechanisms. Cerebral blood flow (CBF) can be calculated using the following formula:
CBF = [Mean Arterial Pressure (MAP) - Intracranial Pressure (ICP)] / Cerebrovascular Resistance (CVR)
The difference between mean arterial pressure and intracranial pressure is known as cerebral perfusion pressure (CPP). Therefore, the formula can also be written as:
CBF = CPP / CVR
Normal CPP ranges from 9.3–12 kPa (70–90 mmHg), while cerebrovascular resistance ranges from 0.16–0.33 kPa (1.2–2.5 mmHg), allowing for proper autoregulation. When increased ICP causes CPP to decrease, the body compensates by dilating blood vessels to reduce vascular resistance, maintaining a stable CBF. However, if ICP continues to rise, reducing CPP below 5.3 kPa (40 mmHg), autoregulation fails, and further vascular dilation cannot compensate. As a result, the value of the formula decreases, leading to a rapid drop in CBF and subsequent cerebral ischemia. When ICP rises to levels close to or exceeding mean arterial pressure, intracranial blood flow nearly ceases entirely, potentially resulting in brain death.
Brain Shift and Brain Herniation
This refers to displacement or herniation of brain structures. Further details are addressed in the context of brain herniation.
Cerebral Edema
Cerebral edema involves water accumulation, which may occur in the extracellular space or inside cells. The former, referred to as vasogenic edema, is commonly seen in conditions such as brain trauma, tumors, and infections. It is primarily caused by increased capillary permeability, leading to fluid retention in the interstitial spaces between neurons and glial cells, resulting in brain volume expansion. The latter, known as cytotoxic edema, arises from metabolic dysfunction in brain cells, causing sodium ions and water to accumulate within neurons and glia. This is often associated with cerebral ischemia and hypoxia. Since both types of edema may coexist or occur sequentially during increased ICP, many cases of cerebral edema are of a mixed type.
Cushing’s Response
A rapid increase in ICP may produce a clinical syndrome known as the Cushing response, characterized by bradycardia, slowed respiration, and elevated blood pressure ("two slows and one high"). This phenomenon is more commonly observed in acute cases of increased ICP, whereas it is less pronounced in chronic conditions.
Gastrointestinal Dysfunction and Digestive Tract Hemorrhage
Some individuals may develop gastrointestinal dysfunction, vomiting, gastrointestinal bleeding, peptic ulceration, or even perforation. These symptoms are related to ischemia of the hypothalamic autonomic centers caused by increased ICP.
Neurogenic Pulmonary Edema
The incidence of neurogenic pulmonary edema in acute cases of increased ICP can reach 5%–10%. This occurs due to compression of the hypothalamus and medulla, leading to heightened alpha-adrenergic nerve activity, increased blood pressure reactivity, excessive left ventricular load, elevated left atrial and pulmonary venous pressure, and increased pulmonary capillary pressure. These changes result in fluid leakage and pulmonary edema, manifested as rapid breathing, wheezing, and copious amounts of frothy, bloody sputum. The mortality rate associated with neurogenic pulmonary edema is relatively high.
Classification
Based on the extent of intracranial pressure elevation, two types can be distinguished:
Diffuse Intracranial Pressure Elevation
This type is caused by a reduction in cranial cavity size or an increase in brain tissue volume. It is characterized by uniformly increased pressure across various parts and compartments of the cranial cavity, with no significant pressure gradient, thus preventing any marked displacement of brain tissue. Conditions such as diffuse meningoencephalitis, diffuse cerebral edema, communicating hydrocephalus, and venous sinus thrombosis fall under this category.
Focal Intracranial Pressure Elevation
This type is caused by localized expansive lesions within the cranial cavity. The lesion site experiences pressure elevation first, leading to compression and displacement of adjacent brain tissue and propagating pressure changes to distant areas. As the pressure gradient between compartments increases, structures such as the ventricles, brainstem, or midline may shift, making this type more prone to cerebral herniation.
Based on the rate of disease progression, three subtypes can be identified:
Acute Intracranial Pressure Elevation
This subtype is commonly observed in acute traumatic brain injuries, intracranial hematomas, and hypertensive cerebral hemorrhages. This subtype is characterized by rapid disease progression, pronounced symptoms and signs of elevated intracranial pressure, and dramatic fluctuations in vital signs (e.g., blood pressure, respiration, pulse, and temperature).
Subacute Intracranial Pressure Elevation
This subtype progresses more slowly than the acute form and is often associated with malignant intracranial tumors, metastases, and various intracranial inflammatory conditions.
Chronic Intracranial Pressure Elevation
This subtype progresses even more gradually and may remain asymptomatic for extended periods. It is commonly seen in slowly growing benign intracranial tumors or chronic subdural hematomas.
Acute, subacute, or chronic intracranial pressure elevation can all lead to cerebral herniation. In cases of herniation, displaced brain tissue is forced into spaces such as the tentorial notch, dural slits, or the foramen magnum, compressing the brainstem and causing critical symptoms. Cerebral herniation exacerbates cerebrospinal fluid (CSF) and blood circulation disturbances, further increasing intracranial pressure and creating a vicious cycle that ultimately leads to death.
Common Diseases Associated with Elevated Intracranial Pressure
Traumatic Brain Injuries
Common causes of elevated intracranial pressure include intracranial hematomas, cerebral contusions with accompanying edema, extensive depressed skull fractures, and traumatic subarachnoid hemorrhages. Less commonly, conditions such as venous sinus thrombosis or fat embolism can also result in elevated intracranial pressure.
Intracranial Tumors
Intracranial pressure elevation occurs in over 80% of cases involving intracranial tumors. The size, location, type, and growth rate of a tumor influence the progression of pressure elevation. Rapidly growing tumors—such as malignant gliomas or metastatic brain tumors—often cause severe cerebral edema, leading to significant pressure elevation over a short period. Tumors located near cerebrospinal fluid pathways may induce obstructive hydrocephalus even when small, resulting in early and pronounced symptoms of intracranial pressure elevation. Conversely, tumors located in the anterior or middle cranial fossa or on the convexity of the brain may cause delayed onset of pressure-related symptoms, even with larger tumor sizes.
Intracranial Infections
Conditions such as meningitis, encephalitis, or brain abscesses can cause elevated intracranial pressure. In late-stage tuberculous meningitis, inflammatory adhesions at the brain base may disrupt CSF circulation, leading to hydrocephalus and increased intracranial pressure.
Cerebrovascular Diseases
Post-hemorrhagic hematoma compression, blood clot obstruction within CSF pathways, or impaired CSF absorption can all result in elevated intracranial pressure. Extensive cerebral infarctions may also cause pressure elevation, with hemorrhagic transformation following infarction further exacerbating this condition.
Parasitic Brain Infections
Elevated intracranial pressure in parasitic brain infections can arise from:
- Localized granulomatous lesions
- Inflammatory adhesions impairing CSF circulation and absorption
- Coexisting cerebral edema
Congenital Cranial Disorders
Congenital hydrocephalus in infants is often due to aberrant development of the cerebral aqueduct, resulting in obstructive hydrocephalus. Conditions such as basilar invagination, Chiari malformation type I, or type II can obstruct CSF circulation in the region of the fourth ventricle or foramen magnum. Craniosynostosis, where premature closure of cranial sutures restricts normal brain growth, may also lead to intracranial pressure elevation.
Benign Intracranial Hypertension (Pseudotumor Cerebri)
This condition frequently manifests in the context of arachnoiditis, with pressure elevation being most marked in arachnoiditis affecting the posterior cranial fossa. Impaired venous return due to thrombosis in the intracranial venous sinuses (such as the superior sagittal or transverse sinuses) may also lead to pressure elevation. Other metabolic disorders, excessive vitamin A intake, drug hypersensitivity, and toxic encephalopathies are additional causes of pressure increase. In most cases, symptoms gradually resolve as the underlying disease improves.
Cerebral Hypoxia
Severe cerebral hypoxia may occur in conditions such as cardiac arrest or significant airway obstruction. Prolonged seizure activity or status asthmaticus (pulmonary encephalopathy) can also lead to severe hypoxia and secondary cerebral edema, resulting in increased intracranial pressure.
Clinical Manifestations
Headache
This is one of the most common symptoms, typically more severe in the early morning or at night, and often localized to the frontal and temporal regions. The intensity of the headache progressively worsens as intracranial pressure increases. Exertion, coughing, bending down, or lowering the head can exacerbate the headache.
Emesis
Severe headaches may be accompanied by nausea and emesis. Emesis can be projectile in nature and, in some cases, may lead to electrolyte imbalance and weight loss.
Papilledema
This is an important objective sign of elevated intracranial pressure, characterized by congestion of the optic disc, blurred margins, loss of the central depression, optic disc swelling, and venous engorgement. Prolonged intracranial pressure elevation may result in pallor of the optic disc, visual impairment, and centripetal narrowing of the visual field, a condition known as secondary optic atrophy. If intracranial pressure elevation is not relieved in a timely manner, recovery of vision becomes difficult, and severe cases may result in blindness.
Headache, emesis, and papilledema are the classic manifestations of elevated intracranial pressure, collectively referred to as the "triad of increased intracranial pressure." However, the onset of these three signs may not occur simultaneously, and any one of them can present as the initial symptom.
Altered Consciousness and Changes in Vital Signs
In the early stages of the condition, altered consciousness may present as drowsiness and slow reactions. Severe cases may present with stupor or coma, accompanied by dilated pupils, loss of pupillary light reflex, cerebral herniation, or decerebrate rigidity. Changes in vital signs include elevated blood pressure, bradycardia, slow respiration, and fever. In the late stages of cerebral herniation, death due to respiratory and circulatory failure is common.
Other Symptoms and Signs
In pediatric patients, symptoms may include an enlarged head, dilation of superficial veins of the scalp and frontal orbital regions, widened or separated cranial sutures, and bulging and tense anterior fontanelles. Percussion of the skull may produce a "cracked pot" sound (MacEwen’s sign).
Diagnosis
A thorough medical history and careful neurological examination are critical for identifying clinically significant information. The presence of the "triad of increased intracranial pressure" confirms the diagnosis. Recurrent vomiting and rapid head circumference growth in children, as well as progressively severe headaches, motor paralysis, and vision loss in adults, should raise suspicion of intracranial pathology. In cases of suspected intracranial pressure elevation, appropriate auxiliary investigations should be considered promptly to facilitate early diagnosis and treatment.
Head CT
This is a fast, precise, and non-invasive diagnostic tool, preferred for initial evaluation of intracranial abnormalities, particularly in emergencies.
Head MRI
This is another non-invasive diagnostic modality that offers higher soft tissue resolution than CT, though it requires a longer examination time and is less effective in visualizing cranial bone structures.
Digital Subtraction Angiography (DSA)
This is useful for diagnosing cerebrovascular diseases and hypervascular intracranial tumors.
Plain Skull X-Ray
This may reveal findings such as suture separation, bone thinning, increased vascular impressions, or foreign bodies, though it is now rarely used as a standalone diagnostic tool.
Lumbar Puncture
This provides information on intracranial pressure but poses risks in patients with elevated intracranial pressure. It may precipitate cerebral herniation, so it must be used cautiously.
Intracranial Pressure Monitoring
Continuous monitoring of intracranial pressure aids in diagnosis, guides drug therapy, and helps determine the timing for surgical intervention.
Treatment Principles
General Management
Patients with elevated intracranial pressure require hospitalization for monitoring.
Continuous observation of consciousness, pupil size, blood pressure, respiration, pulse, and temperature changes is essential.
For patients meeting the criteria for intracranial pressure monitoring, management may benefit from guidance based on these measurements.
Individuals experiencing frequent vomiting should temporarily discontinue eating to reduce the risk of aspiration pneumonia.
Fluid administration needs to be carefully regulated; excessive fluid can worsen intracranial pressure elevation, while insufficient fluid may lead to blood concentration.
Mild laxatives may be administered to facilitate bowel movements while avoiding strong efforts during defecation. High enemas should be avoided to prevent sudden increases in intracranial pressure.
For comatose patients or those with difficulty expectorating, tracheotomy may be considered to improve airway patency and minimize further increases in intracranial pressure.
Etiological Treatment
For intracranial space-occupying lesions without surgical contraindications, resection of the lesion may be prioritized.
In cases of hydrocephalus, cerebrospinal fluid drainage may be performed externally, or redirected to the subarachnoid space, peritoneal cavity, or atrium, as appropriate.
Acute cerebral herniation requires urgent intervention, including emergency rescue or surgical measures.
Pharmacological Treatment
Applicable in cases where the underlying cause remains unidentified or where non-surgical management is necessary despite an identified cause. Commonly used agents include 20% mannitol, furosemide, hypertonic saline, and intravenous infusion of 20% human serum albumin.
Glucocorticoids
Medications such as dexamethasone, hydrocortisone, and prednisone can reduce cerebral edema and alleviate intracranial pressure. However, glucocorticoids do not show definitive efficacy for cerebral edema resulting from traumatic brain injury.
Barbiturate Therapy
High-dose administration of sodium pentobarbital or thiopental can lower cerebral metabolism, reduce cerebral blood flow, decrease oxygen consumption, and enhance brain tolerance to hypoxia, effectively reducing intracranial pressure. Monitoring of blood drug concentrations, cerebral blood flow, and cerebral metabolism is recommended during therapy. However, clinical studies have shown that barbiturate therapy does not improve patient prognosis.
Hyperventilation
A reduction of 1 mmHg in arterial partial pressure of CO2 can lead to a 2% reduction in cerebral blood flow, which subsequently decreases intracranial pressure.
Symptomatic Treatment
Analgesics may be administered to alleviate headaches, although morphine and pethidine should be avoided to prevent suppression of the respiratory center.
Anticonvulsant therapy is indicated for patients experiencing seizures.
Sedatives can be used to address agitation, provided intracranial pressure progression, airway obstruction, and defecation issues have been ruled out as contributing factors.