Epidemic Parotitis (Mumps)
If a pregnant woman contracts mumps, the newborn may exhibit congenital ocular abnormalities such as microphthalmos, microcornea, corneal opacities, congenital cataracts, nystagmus, and optic atrophy.
When children contract mumps, ocular manifestations may include follicular conjunctivitis, keratitis, scleritis, iritis or uveitis, glaucoma, extraocular muscle palsy, dacryoadenitis, and optic neuritis. Optic neuritis is the most common ocular complication associated with meningitis and encephalitis in this condition and is typically bilateral.
Acute Bacillary Dysentery
Acute bacillary dysentery may lead to dehydration, causing dryness of the eyelid skin. Cortical blindness may occur as a result of high fever or toxin exposure. Retinal artery spasms and retinal edema may be observed in cases of toxic dysentery. Some children may additionally develop conjunctivitis, iridocyclitis, or optic neuritis.
Retinopathy of Prematurity (ROP)
Retinopathy of Prematurity (ROP) refers to a retinal disorder that occurs in infants born before 36 weeks of gestation, with a birth weight under 2,000 grams, and who have a history of oxygen supplementation after birth. Its incidence is approximately 60%. For those born at an earlier gestational age or with an even lower birth weight, the incidence increases to 66–82%. In developed countries, ROP is a major cause of pediatric blindness. ROP typically emerges at a corrected gestational age (gestational weeks plus postnatal weeks) of 32 weeks, with threshold disease appearing around 37 weeks. Early screening and treatment can halt the progression of the disease.
Etiology
The incomplete vascularization of the retina makes it susceptible to vascular constriction and neovascular proliferation due to oxygen exposure. Normally, retinal vasculature reaches the nasal edge by around 36 weeks of gestation and the temporal edge by 40 weeks. Exposure to high concentrations of oxygen during this period may lead to damage to endothelial cells in the capillaries, vascular occlusion, and subsequent stimulation of fibrovascular proliferation.
Clinical Signs and Staging
ROP Location Classification by Zone
ROP is classified into three zones based on its location:
- Zone I: A circular area centered on the optic disc, with a radius twice the distance between the optic disc center and the foveal center.
- Zone II: A circular area centered on the optic disc, with a radius extending to the nasal ora serrata, excluding Zone I. Within Zone II, there is a posterior segment (posterior Zone II) extending approximately two optic disc diameters from the temporal edge of Zone I near the macula. Diseases in this posterior Zone II are more concerning compared to diseases in the peripheral Zone II.
- Zone III: The remaining peripheral area beyond Zone II.
The closer the lesion is to the posterior pole (Zone I), the higher the risk of progression.
Disease Severity Staging
The disease can be classified into:
- Stage 1: A demarcation line appears between the vascularized and non-vascularized retina, which is white in color. Peripheral retinal vessels beyond the white line may show mild dilation and tortuosity.
- Stage 2: The demarcation line becomes elevated, forming a ridge-like structure with a white to pink appearance. Small neovascular buds on the retinal surface, referred to as "popcorn," may appear behind the ridge but do not constitute Stage 3.
- Stage 3: Extraretinal neovascular proliferation grows over the ridge and extends into the vitreous. The condition may occur in Zone I or Zone II. A ridge or demarcation line may not always be visible, yet the diagnosis can still be made.
- Stage 4: Partial retinal detachment occurs as fibrous proliferation pulls on the retina. This may lead to macular displacement, macular vascular arch straightening, and other changes caused by the traction of peripheral fibrous membranes.
- Stage 5: Total retinal detachment is present. In late-stage disease, the anterior chamber becomes shallow or disappears, and secondary complications such as glaucoma, corneal degeneration, and phthisis bulbi may arise.
- Plus Disease: At least two quadrants of the retina show dilation and tortuosity of posterior retinal blood vessels. Severe plus disease may also involve iris vascular congestion or dilation, difficulty in pupil dilation, and vitreous opacities. The presence of plus disease signals the severity of active diseases. When plus disease is present, it is denoted with a "+" beside the stage number (e.g., Stage 3+).
- Pre-Plus Disease: Retinal blood vessel dilation and tortuosity are abnormal but do not meet the criteria for plus disease.
- Threshold Disease: Defined as Stage 3+ disease in Zone I or Zone II involving at least five contiguous clock hours or eight cumulative clock hours. It requires treatment.
- Pre-Threshold Disease: Significant ROP findings that do not yet meet the severity criteria for threshold disease. It is further divided into "Type 1 Pre-Threshold Disease" and "Type 2 Pre-Threshold Disease."
- Aggressive Posterior ROP (AP-ROP): A rapidly progressing form of ROP that occurs in Zone I or posterior Zone II, often involving four quadrants. The disease appears flat, with the ridge not prominent, and vascular shunting occurring both at the junction of vascularized and non-vascularized retina and within the retina.
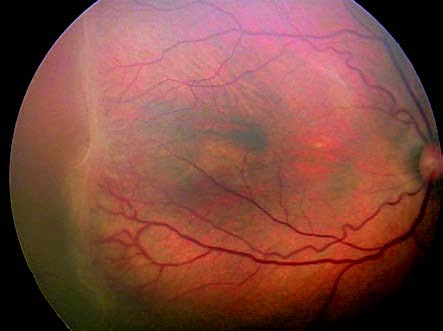
Figure 1 Retinopathy of prematurity stage 3 + plus
ROP Classification Based on Disease Type
This disease can be divided into:
- Type 1 ROP: Any disease in Zone I with plus disease; Stage 3 in Zone I, with or without plus disease; Stage 2 in Zone II with plus disease; Stage 3 in Zone II with plus disease. Type 1 ROP meets criteria for treatment and is considered an indication for intervention within 24–48 hours.
- Type 2 ROP: Stage 1 or Stage 2 disease in Zone I; Stage 3 disease in Zone II. Type 2 ROP is considered an observational condition and may be managed by regular monitoring.
Key Diagnostic Points
Diagnostic considerations include:
- Medical History: A history of preterm birth and low birth weight is relevant.
- Clinical Manifestations: The presence of a demarcation line between vascularized and non-vascularized retina in early stages of ROP is a characteristic feature. Proliferative changes at the demarcation line, abnormal retinal vascular development, varying degrees of tractional retinal detachment, and late-stage changes should raise suspicion for ROP.
Screening Criteria
Screening Guidelines Based on Birthweight and Gestational Age
Fundus examination should be conducted for preterm infants with a birth weight below 2,000g or a gestational age below 32 weeks, with follow-up until peripheral retinal vascularization is complete. Screening can be expanded for infants with severe systemic illness, extended oxygen therapy, or high-risk assessments from pediatricians.
Time for Initial Screening
The first examination should take place at 4–6 weeks after birth or at a corrected gestational age of 31–32 weeks.
Timeframe for Intervention
For confirmed threshold disease or Type 1 pre-threshold disease, treatment should ideally begin within 72 hours. Referral to a higher-level facility is needed if treatment is unavailable locally.
Requirements for Personnel
Screening should be performed by experienced ophthalmologists with relevant knowledge.
Screening Techniques
Mydriasis should be appropriately induced for examination. Indirect ophthalmoscopy is recommended, although wide-field fundus photography may also be used. Scleral depression can be utilized during the examination, and a minimum of two examinations is advised.
Screening Intervals
This disease should be screened with the following intervals:
- Zone I with no ROP or with Stage 1 or Stage 2 ROP: Weekly examination is recommended.
- Regressing ROP in Zone I: Examination intervals may be extended to 1–2 weeks.
- Stage 2 or Stage 3 disease in Zone II: Weekly examinations are recommended.
- Stage 1 disease in Zone II: Examination intervals may be 1–2 weeks.
- Stage 1 in Zone II or Zone III, or no ROP in Zone III: Follow-up every 2–3 weeks is sufficient.
Criteria for Terminating Screening
Follow-up can be stopped if any of the following conditions are met:
- Retinal vascularization reaches the ora serrata nasally and within one optic disc diameter of the ora temporally.
- Corrected gestational age reaches 45 weeks, with no pre-threshold or threshold disease, and retinal vascularization reaches Zone III.
- Retinal disease shows regression.
Treatment Principles
Regular monitoring is required for Stage 1 or Stage 2 disease in Zone III.
Treatment options for pre-threshold or threshold disease include intravitreal anti-VEGF injection, laser therapy under indirect ophthalmoscopy, or cryotherapy.
Surgical intervention may be appropriate for Stage 4 or Stage 5 disease.