Chemical burns refer to tissue damage caused by chemical solutions, powders, or gases coming into contact with the eye. They often occur in chemical plants, laboratories, or construction sites. Acid and alkali burns are the most common types, and they are medical emergencies requiring immediate attention.
Mechanisms of Injury
The mechanisms of injury differ between acid and alkali burns:
- Acid Burns (Acid Burn Injuries): Acids cause protein coagulation. At lower concentrations, they result in irritation, while strong acids lead to coagulative necrosis of tissue proteins. The coagulated proteins form a barrier that can prevent deeper penetration, resulting in relatively less severe tissue damage.
- Alkali Burns (Alkali Burn Injuries): Commonly caused by substances such as sodium hydroxide, quicklime, or ammonia. Alkalis are capable of dissolving fats and proteins, allowing rapid penetration into deeper tissues and even into the globe. These injuries are typically more severe due to the resultant cell lysis and necrosis.
Clinical Presentation and Complications
Based on tissue response, acid and alkali burns can be classified into mild, moderate, and severe injuries.
- Mild Burns: Usually caused by weak acids or diluted weak alkalis. These burns manifest as mild eyelid and conjunctival hyperemia and edema, with punctate corneal epithelial erosion or edema. Edema resolves within a few days, and epithelial repair occurs without scarring or significant complications. Visual function is typically unaffected.
- Moderate Burns: Often caused by strong acids or more diluted alkalis. These burns can lead to blistering or erosion of the eyelid skin, conjunctival edema, and localized areas of ischemic necrosis. The cornea may develop significant opacification or edema, with complete epithelial loss or the formation of a white, coagulated layer. After healing, corneal opacity may remain, leading to vision impairment.
- Severe Burns: Mostly caused by strong alkalis. Extensive ischemic necrosis of the conjunctiva occurs, presenting as grayish-white opacity. The cornea can appear grayish-white or porcelain-like. Chemotactic factors released from necrotic tissues attract large numbers of neutrophils that release collagenase, leading to corneal stromal dissolution, and complications such as corneal ulcers or perforation. Alkalis rapidly penetrate the anterior chamber, causing conditions such as uveitis, secondary glaucoma, and cataracts. Corneal ulcers may heal to form corneal leukomas, and corneal perforations may heal to create anterior adhesions, corneal staphylomas, or phthisis bulbi.
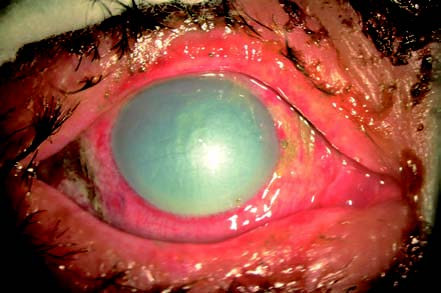
Figure 1 Alkali chemical burn
Day 3 after an alkali burn to the right eye, showing burned, scabbed eyelid skin; conjunctival hyperemia and localized necrosis; and porcelain-white, edematous, and cloudy cornea.
Epithelial defects in the conjunctiva during healing can lead to symblepharon and pseudopterygium, ultimately causing loss of visual function or the globe itself. Elevated intraocular pressure (IOP) in alkali burns may be caused by immediate scleral contraction and trabecular damage, leading to rapid IOP elevation. After 2–4 hours, prostaglandin release can cause another rise in IOP. Corneal opacity often makes it difficult to measure IOP.
In addition, burns to the eyelid and lacrimal system can cause complications such as eyelid deformities, incomplete eyelid closure, and epiphora.
Emergency Management and Treatment
Emergency Management
The primary step in managing acid and alkali burns involves immediate and thorough irrigation to minimize tissue damage. Irrigation with a copious amount of water or any available liquid source can significantly reduce the extent of injury. The process should involve everting the eyelids and rotating the globe to ensure clearance of chemical substances from the fornices and conjunctival sac. Irrigation is typically recommended for at least 30 minutes. On arrival at a medical facility, further irrigation may be performed based on the time elapsed from the injury, along with examination for residual foreign materials in the conjunctival sac. Anterior chamber paracentesis may also be performed to reduce intraocular damage.
Subsequent Treatment
Early Treatment
Infection Control
Administration of topical or systemic antibiotics is used to prevent infection. Regular dilation of the pupil with 1% atropine may help prevent posterior synechiae.
Inflammation Suppression
Corticosteroids are administered either locally or systemically to suppress inflammation and neovascularization. However, steroids should be discontinued 2–3 weeks post-injury if there is a risk of corneal dissolution.
Corneal Healing
Eye drops containing autologous serum or growth factors may promote corneal healing. For lime burns, 0.5% EDTA can chelate calcium deposits. Antiglaucoma medications are used to maintain low IOP during the first two weeks. Collagenase activity, which contributes to corneal dissolution, can be suppressed using collagenase inhibitors (e.g., topical 2.5%–5% cysteine eye drops or systemic tetracyclines).
Surgical Interventions
In cases of severe conjunctival or corneal epithelial necrosis, excision of necrotic tissue during the early stages may prevent complications like symblepharon. Severe cases involving corneal thinning or dissolution within two weeks may necessitate full-thickness corneal lamellar transplantation with limbal epithelial cell preservation to rescue the globe. Amniotic membrane grafting, limbal stem cell transplantation, autologous oral mucosal grafting, or contralateral conjunctival transplantation may be performed as needed. Adhesions between the conjunctiva and eyelids can be managed using spacers or glass rods during dressing changes.
Late Treatment
Late-stage treatment focuses on managing complications, such as surgical correction of ectropion or symblepharon and performing keratoplasty. Secondary glaucoma may require medical treatment for IOP control or surgical interventions such as ciliary body cryotherapy or laser photocoagulation (810 nm) to reduce IOP.