Intraocular foreign bodies (IOFBs) are a type of ocular trauma that poses a serious threat to vision. Any open injury to the eye or orbit warrants suspicion and evaluation for the presence of foreign bodies. Metal-on-metal impact is the most common mechanism of injury. Factors contributing to damage from foreign bodies include mechanical destruction, chemical and toxic reactions, and secondary infections. In addition to the penetrating injury, foreign bodies can cause specific additional harm.
Pathology and Clinical Manifestations
The ocular response to an intraocular foreign body depends on its chemical composition, location, and whether infection is present.
General Considerations
Inert and sterile foreign bodies, such as stone, sand, glass, ceramics, and plastic, are generally well-tolerated. Reactive foreign bodies, such as iron, copper, aluminum, and zinc, are more common. Aluminum and zinc cause mild inflammation and may become encapsulated; however, large foreign bodies can incite inflammation, leading to cellular proliferation, tractional retinal detachment, and eventual phthisis bulbi. Foreign bodies can also migrate within the eye.
Ocular Siderosis
The mechanism of damage caused by intraocular iron ions is thought to involve rapid oxidation and diffusion of iron ions upon contact with the vitreous or intraocular tissues. This triggers the Haber-Weiss reaction, generating strong oxidizing agents such as hydroxyl radicals, superoxide radicals, and hydrogen peroxide. These result in lipid peroxidation, cellular membrane damage, and enzyme inactivation, leading to severe structural and functional impairment.
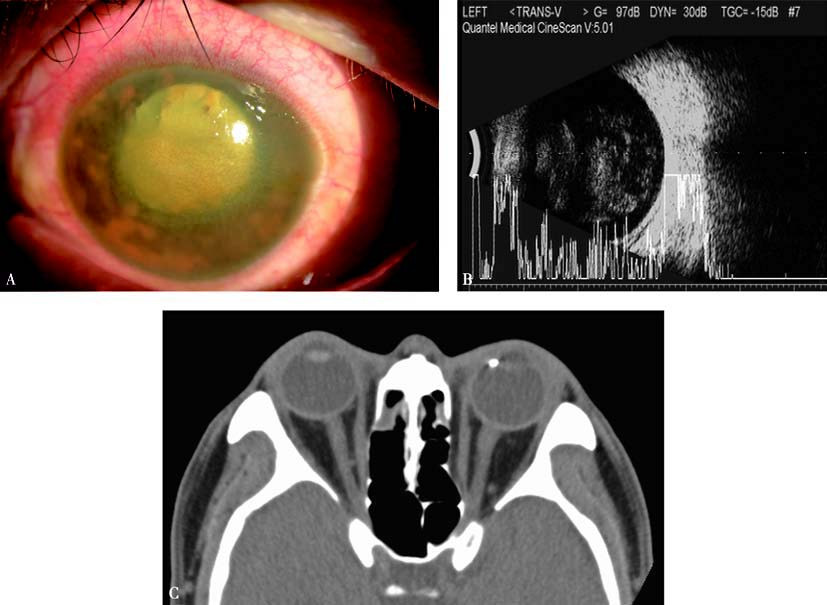
Figure 1 Ocular siderosis
A. Anterior segment of the left eye shows mild corneal opacity, iris heterochromia with rust-colored deposits on the iris surface, dilated pupil, and lens opacity.
B. A/B-scan ultrasound demonstrates vitreous opacities.
C. CT imaging shows a metallic foreign body near the nasal-side ciliary body of the left eye.
Iron deposition is most common in epithelial tissues, including the pupillary sphincter and dilator muscles, non-pigmented ciliary epithelium, lens epithelium, and retina. Photoreceptors and retinal pigment epithelial cells are particularly sensitive to iron deposition.
Symptoms include night blindness, concentric visual field loss, and eventual blindness.
Clinical signs include rust-colored deposition in the corneal stroma, heterochromia of the iris, dilated and sluggish pupils, brown deposits on the anterior lens capsule, cataracts, vitreous opacities, and pigment proliferation in the peripheral retina (early stages) or diffusely (late stages). Retinal vessels may show narrowing, and the optic disc may appear pale or atrophic. Iron ion accumulation in the trabecular meshwork can lead to secondary open-angle glaucoma.
Electroretinogram (ERG) findings may include a very early increase in the a-wave amplitude, initially normal b-waves, followed by gradual b-wave reduction, and eventual disappearance of both waves.
Ocular Chalcosis
Pure copper exhibits significant toxicity and can cause acute chalcosis and severe inflammation, warranting immediate removal. Copper alloys containing less than 85% copper may result in chronic chalcosis. Copper ions preferentially bind to membrane-like structures, resulting in characteristic clinical manifestations, such as copper deposition in Descemet's membrane (Kayser-Fleischer ring), greenish granular deposits in the aqueous humor, green discoloration of the iris, sunflower cataract, brown-red vitreous opacities with fibrous bands, and metallic deposits on retinal vessels and in the macular region. Once copper diffuses throughout the eye, removal of the foreign body does not mitigate the damage.
Diagnosis
A history of injury, such as metal-on-metal impact, stone strikes, blast injuries, or shattered windshield glass during traffic accidents, raises suspicion for retained IOFBs. High-velocity small metal fragments, often expelled from hammers or machines, are particularly prone to being overlooked.
Clinical Features
Signs of penetrating injury are typically present, and the discovery of a wound is a key diagnostic indicator. For instance, a linear corneal wound or full-thickness scar accompanied by iris perforation and localized lens opacities suggests intraocular foreign body entry. Scleral wounds are harder to detect. If the optical media remain clear, foreign bodies may be directly visualized using a slit-lamp biomicroscope or ophthalmoscope. Gonioscopy or fundus examination with a contact or three-mirror lens may detect foreign bodies hidden in the anterior chamber angle or peripheral retina. The retinal toxicity of the foreign body can be assessed using ERG testing.
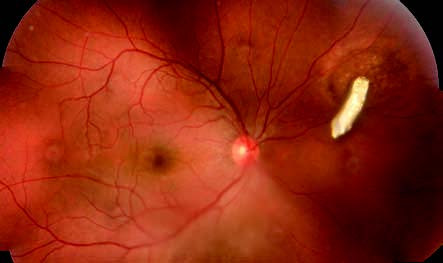
Figure 2 Retinal iron foreign body
A reflective metallic foreign body can be observed on the surface of the retina, located 3 disc diameters (DD) superior-nasal to the optic disc of the right eye. The surrounding retina appears to be affected.
Imaging Investigations
Imaging modalities include X-ray radiography, B-scan ultrasonography, ultrasound biomicroscopy (UBM), and computed tomography (CT). Each method has its advantages and limitations. Magnetic resonance imaging (MRI) is contraindicated for evaluating magnetic foreign bodies.
Treatment
Intraocular foreign bodies generally require early surgical removal to restore ocular structure and visual function. The surgical approach depends on factors such as the size and location of the foreign body (e.g., within the vitreous cavity or embedded in the retina or other structures), its characteristics (e.g., magnetic or non-magnetic, encapsulated or not), and the presence of ocular complications (e.g., reduced media clarity that obstructs visualization of the foreign body, intraocular hemorrhage, or infection).
Foreign Bodies in the Anterior Chamber and Iris
Foreign bodies can be removed through a corneal limbal incision made either in the direction of or opposite to the location of the foreign body. Magnetic foreign bodies can be extracted using an electromagnet, while non-magnetic foreign bodies can be removed with forceps.
Foreign Bodies in the Lens
If the lens remains mostly transparent, immediate surgery may not be required. If the lens becomes significantly opaque, the foreign body and lens may be removed together.
Foreign Bodies in the Posterior Segment of the Eye
Small foreign bodies that are completely encapsulated within the scleral wall may not require removal. For very small iron foreign bodies left in situ, repeated ERG examinations may provide useful information. If there is a reduction in the b-wave amplitude, removal of the foreign body is recommended.
Depending on the circumstances, posterior segment foreign bodies can be removed via an external approach or through vitreoretinal surgery. Small, visible magnetic foreign bodies within the vitreous that are unencapsulated and not associated with retinal complications can be extracted using an electromagnet through the pars plana. In other cases, such as large foreign bodies, those that are encapsulated, adhered, or non-magnetic, vitreoretinal surgery is required. This procedure also addresses associated intraocular complications such as vitreous hemorrhage or retinal detachment. Larger foreign bodies may be removed through a corneoscleral incision or the original entry wound to minimize damage to peripheral retinal tissue.