Ruptured globe is caused by severe blunt trauma. Common rupture sites include the limbus and areas beneath the extraocular muscles. Rupture sites often exhibit prolapse or incarceration of intraocular tissues. Intraocular pressure (IOP) is typically reduced, but it may also remain normal or even increase. Other clinical features include hyphema or vitreous hemorrhage, subconjunctival hemorrhage and edema, corneal deformation, restricted ocular motility in the direction of the rupture, and vision reduced to light perception or worse. CT imaging or B-scan ultrasonography may reveal signs such as discontinuity of the globe wall, globe deformation, volume shrinkage, shortening of axial length, or structural damage within the eye.
In some patients, particularly those with posterior rupture located beneath extraocular muscles or in the posterior sclera, detection can be challenging. Factors such as an intact conjunctiva or extensive subconjunctival hemorrhage covering the rupture site can mask the injury, making external examination unreliable. This condition is referred to as "occult scleral rupture," a special type of globe rupture. Its clinical characteristics include:
- A history of severe blunt ocular trauma.
- Vision reduced to light perception or worse.
- Subconjunctival hemorrhage and edema.
- Low intraocular pressure.
- Varying degrees of hyphema.
- Impaired ocular motility.
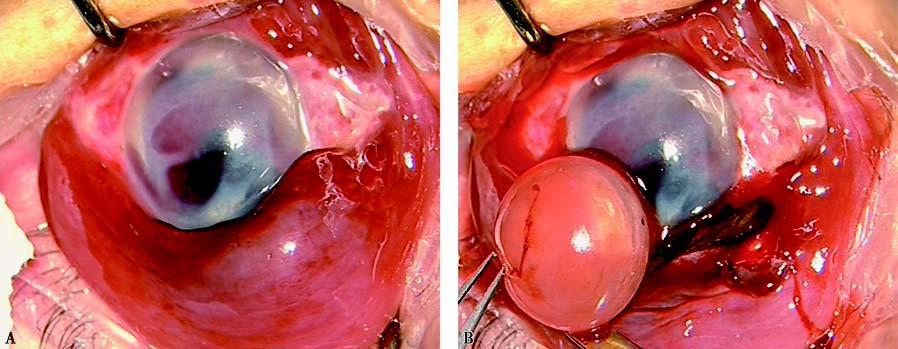
Figure 1 Occult scleral rupture
(A) Subconjunctival hemorrhage and edema in the left eye, corneal edema and opacity, and hyphema in the anterior chamber.
(B) Surgical exploration revealed a scleral wound posterior to the limbus, extending more than 8mm posteriorly. The lens (indicated by forceps) is dislocated, and both the uvea and vitreous are incarcerated in the wound.
When 4–5 of these clinical signs are present, the likelihood of a scleral rupture is extremely high. Damage to intraocular structures, such as lens dislocation, vitreous hemorrhage, or retinal detachment, may serve as vital diagnostic indicators, guide treatment strategies, and aid in prognosis assessment. Combining clinical evaluation with imaging studies, including A/B-scan ultrasonography and CT, can reduce the risk of misdiagnosis and missed diagnoses.
Treatment
Emergency management follows the general protocols for ocular trauma. Definitive care often involves a two-stage surgical process. The initial procedure consists of emergency primary repair of the globe, followed by administration of antibiotics and corticosteroids to control infection and trauma-related inflammatory responses. For suspected occult scleral rupture, surgical exploration is used to avoid misdiagnosis. If a rupture is identified, suturing is performed. Subsequent A/B-scan ultrasonography and visual electrophysiological assessments guide additional treatment. Depending on the specific condition, vitrectomy may be performed 1–2 weeks after the initial repair surgery, potentially preserving the globe's structural integrity and some functional vision. Primary enucleation is generally avoided unless the globe is so severely damaged that it cannot be repaired.