Choroidal Rupture
This condition can be singular or multiple and frequently occurs in the posterior pole or around the optic disc, appearing as an arc-shaped rupture with its concave side facing the optic disc. In the early stages after injury, the rupture site is often obscured by hemorrhage. Once the hemorrhage resolves, yellowish-white scars become visible. Ruptures extending to the central macula significantly impair visual acuity, and the rupture site may develop choroidal neovascularization. No effective treatment exists.
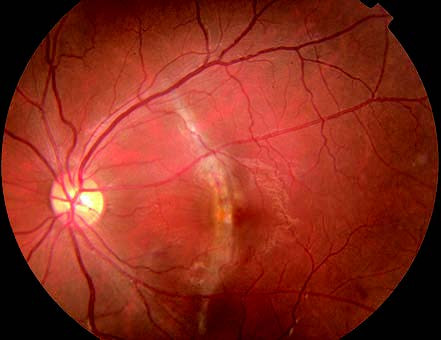
Figure 1 Choroidal rupture
A yellowish-white arc-shaped scar can be seen crossing the macular region in the left fundus.
Retinal Commotion and Contusion
This refers to transient retinal edema in the posterior pole caused by trauma, resulting in whitening of the retina and decreased visual acuity. Shockwaves from the site of injury damage the outer retinal layers, disrupt the retinal pigment epithelium, impair barrier functions, and lead to extracellular edema, causing retinal opacity and a decline in visual acuity, often to levels below 0.1. This condition presents two main outcomes:
- In some cases, the edema resolves within 3–4 weeks with good visual recovery, a condition described as "commotio retinae."
- In other cases, notable photoreceptor damage, outer retinal degeneration and necrosis, pigment disturbance in the macula, and significant visual impairment occur, referred to as "retinal contusion." Severe cases may involve retinal hemorrhages.
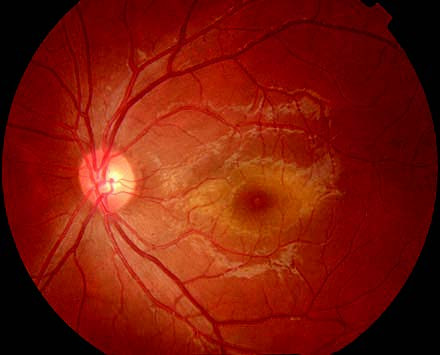
Figure 2 Retinal commotion
Grey-white opacity is present in the macular region following blunt trauma to the left eye.
Treatment during the early stages of injury may involve high-dose corticosteroids to potentially mitigate retinal edema-related damage. The efficacy of neurotrophic drugs, vasodilators, and vitamin-based treatments remains uncertain.
Traumatic Macular Hole
This condition is usually characterized by full-thickness macular holes caused by localized contusion necrosis and vitreoretinal traction. It may occur immediately or develop following macular edema, choroidal rupture, subretinal hemorrhage, or posterior vitreous detachment. A small number of cases may result in retinal detachment.
Traumatic macular holes have a low likelihood of causing retinal detachment and can initially be monitored clinically. Surgical intervention is required if retinal detachment occurs, but postoperative vision typically shows limited improvement.
Ora Serrata Dialysis
This presentation is a common form of retinal detachment due to ocular trauma, often occurring in the superonasal or inferotemporal quadrants. Retinal tears may also develop in other peripheral areas as a result of trauma, potentially leading to retinal detachment.
Treatment for ora serrata dialysis or peripheral retinal tears involves scleral buckling surgery. Complex cases, such as those involving giant retinal tears, vitreous hemorrhage, or traumatic proliferative vitreoretinopathy, require vitrectomy.