Optic glioma originates from the glial cells of the optic nerve and is the most common optic nerve tumor. It frequently occurs in children and adolescents, with most cases being low-grade gliomas.
Clinical Manifestations
Progressive vision decline is the most common initial and primary symptom. As the tumor enlarges, it often presents as painless, progressive proptosis. Fundoscopic examination may reveal optic disc edema, hemorrhage, or pallor, along with optic atrophy. When the tumor extends to the optic chiasm or intracranial structures, symptoms such as precocious puberty, hydrocephalus, and elevated intracranial pressure may develop. Some patients may have associated Neurofibromatosis Type 1 (NF1), which presents with skin café-au-lait spots and iris Lisch nodules. CT typically shows tortuous thickening of the optic nerve, with a spindle-shaped or oval enlargement. The tumor may feature cystic degeneration, and when extending intracranially, widening of the optic canal may also be observed, with the optic nerve appearing spindle-shaped or doughnut-shaped. MRI reveals a clearly delineated tumor with enlargement. The signal appears isointense or slightly hypointense on T1-weighted imaging (T1WI) and hyperintense on T2-weighted imaging (T2WI). Contrast enhancement demonstrates various degrees of enhancement, with no clear demarcation between the tumor and normal optic nerve.

Figure 1 CT imaging of right optic glioma
Axial CT shows tortuous thickening of the right optic nerve, with oval-shaped enlargement and widening of the bony optic canal.
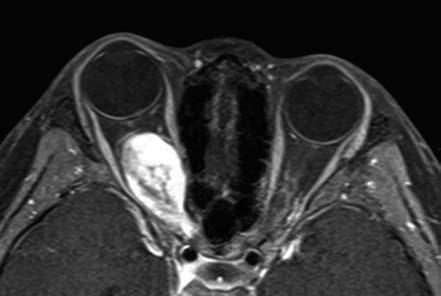
Figure 2 MRI of right optic glioma
Enhanced T1-weighted MRI in the axial view demonstrates irregular thickening and enlargement of the right optic nerve with inhomogeneous enhancement.
Treatment
For patients with stable vision, close clinical observation is indicated. Patients experiencing progressive visual impairment may receive precise radiotherapy, including stereotactic or three-dimensional conformal radiotherapy. In cases of severe proptosis accompanied by vision loss or uncontrolled tumor progression toward the optic chiasm and intracranial structures, surgical resection may be considered.