Uveal melanoma (UM) is the most common primary intraocular malignant tumor in adults. Based on its location, UM can be classified into choroidal melanoma (90%), ciliary body melanoma (6%), and iris melanoma (4%). Approximately 50% of UM patients eventually develop distant metastases, most commonly in the liver. Once distant metastases occur, the median survival time is less than one year.
Pathogenesis
UM is mainly associated with genetic mutations and chromosomal abnormalities, including gain-of-function mutations in G-protein alpha subunit q (GNAQ) and G-protein alpha subunit 11 (GNA11), BRCA1-associated protein 1 (BAP1) loss, monosomy of chromosome 3, and amplification of the long arm of chromosome 8. In addition, epigenetic dysregulation plays an important role in the development and progression of UM.
Clinical Manifestations
The symptoms of choroidal melanoma are closely related to the size and location of the tumor. Tumors located in the macular region may cause early symptoms such as distortion of vision or reduced visual acuity. Tumors in the peripheral retina present fewer noticeable symptoms during the early stages. Based on tumor growth patterns, UM can appear as either localized or diffuse, with localized forms being more common. Localized tumors often present as hemispherical or mushroom-shaped masses protruding towards the vitreous cavity. Diffuse tumors spread horizontally along the choroid, leading to generalized thickening of the choroid without significant elevation. As the tumor progresses, it may result in exudative retinal detachment, secondary glaucoma, or vitreous hemorrhage.
Ciliary body melanoma is often hidden behind the iris in its early stages and is usually asymptomatic. It is often discovered after lens displacement, retinal detachment, or scleral extension. Iris melanoma is commonly identified through noticeable changes in iris pigmentation (heterochromia) or pupil deformation.
Diagnosis
The diagnosis of UM is primarily clinical and is based on a thorough medical history, along with examinations such as scleral transillumination, anterior segment and fundus photography, ocular ultrasound, fundus fluorescein angiography (FFA), indocyanine green angiography (ICGA), magnetic resonance imaging (MRI), and systemic evaluations. In most cases, a clinical diagnosis can be established.
Ocular Ultrasound
On A-scan, choroidal melanoma typically exhibits a moderately low internal reflectivity with smooth attenuation. Blood vessel pulsations within the tumor may produce sharp peaks of rapid motion. On B-scan, typical choroidal melanomas appear as dome-shaped or mushroom-shaped elevated lesions with low-to-moderate internal echogenicity. Subretinal fluid, a "choroidal excavation sign," and choroidal depressions may also be observed. Ultrasound biomicroscopy (UBM) is often employed for examining iris and ciliary body tumors, allowing for detailed evaluation of the lesion and assessment of adjacent tissue invasion.
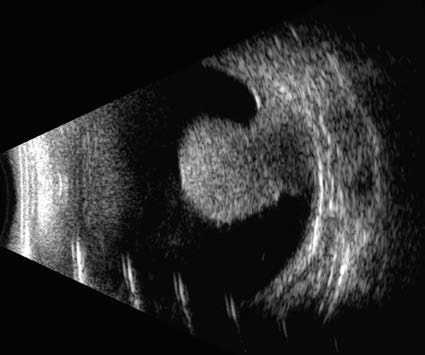
Figure 1 B-scan ultrasound imaging of choroidal melanoma in the right eye
A mushroom-shaped elevated lesion is observed in the posterior segment of the right eye, measuring 11.8 mm × 10.8 mm × 10.0 mm. The lesion exhibits medium-to-low internal echogenicity, accompanied by a "choroidal excavation sign" and surrounding areas of strong, band-like echoes, consistent with choroidal melanoma with retinal detachment.
Anterior Segment and Fundus Photography
These methods provide objective documentation of tumor location, morphology, pigmentation, vascular characteristics, and any changes in the lens or pupil. In cases of ciliary body and choroidal melanoma, pupil dilation is required to facilitate detailed examination. Peripheral retinal status is also documented to determine the extent and location of tumor involvement and associated exudative retinal detachment.

Figure 2 Fundus photograph and FFA of choroidal melanoma in the right eye
A. The fundus image shows a subretinal brownish, round, elevated lesion in the superotemporal retina extending into the macular area, with orange pigment visible on its surface.
B. The corresponding FFA image reveals progressive fluorescein leakage over time. In the late phase of angiography, the lesion exhibits diffuse hyperfluorescence, with dilated blood vessels visible within the tumor.
FFA and ICGA
On FFA, UM typically presents as patchy hyperfluorescence in the early phase, with diffuse vascular leakage visible in the late phase due to persistent leakage from tumor blood vessels. On ICGA, if the tumor has not breached Bruch's membrane, the choroidal vessels within the tumor are undetectable. However, if the tumor breaches Bruch's membrane, the ICGA images may reveal irregular and disrupted large retinal vessels overlying the tumor, along with various abnormal tumor-associated vascular structures.
OCT
Compared to ultrasound, OCT is more advantageous for measuring small choroidal melanomas. Anterior segment OCT is suitable for evaluating iris melanomas.
MRI
Classic UM appears as a hyperintense signal on T1-weighted imaging and a hypointense signal on T2-weighted imaging, with significant enhancement on post-contrast scans. MRI also provides valuable information regarding possible extrascleral extension of the tumor.
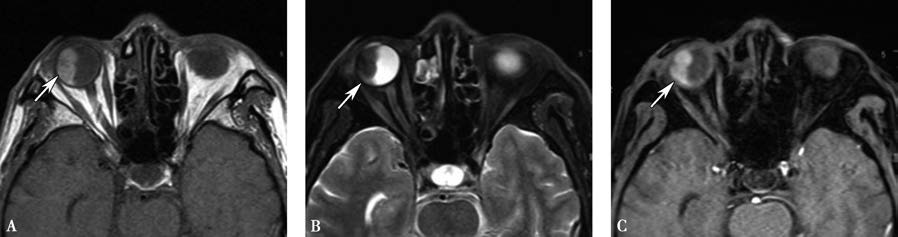
Figure 3 MRI of uveal melanoma
A. T1WI shows an elliptical intraocular mass in the right eye with high signal intensity.
B. T2WI shows the intraocular mass as hypointense.
C. Post-contrast imaging reveals the intraocular lesion with irregular enhancement in the right eye.
PET-CT
PET-CT has high sensitivity and diagnostic value for detecting and monitoring systemic metastases in UM patients.
Differential Diagnosis
Common differential diagnoses include choroidal hemangioma, choroidal metastatic carcinoma, melanocytoma, choroidal nevus, peripheral exudative hemorrhagic chorioretinopathy, and congenital hypertrophy of the retinal pigment epithelium (CHRPE). When clinical presentations are atypical, intraocular biopsy can help achieve a definitive diagnosis.
Choroidal Hemangioma
This is a benign vascular tumor of the choroid. Typical fundus findings include a well-defined, smooth, orange-red, round, elevated lesion in the posterior pole, often accompanied by exudative retinal detachment. On ICGA, the tumor typically shows early intense hyperfluorescence, followed by rapid dye clearance with a mottled fluorescence appearance in later phases. On MRI, choroidal hemangioma typically presents as high signal intensity on T1WI, isointensity on T2WI, and exhibits marked enhancement after contrast administration. CDI findings often show a high-velocity, low-resistance flow spectrum.
Choroidal Metastatic Carcinoma
This condition often lacks significant pigment deposition and typically has irregular borders. On A-scan, metastatic choroidal carcinoma usually shows reflectivity that is significantly higher than that of UM. B-scan findings typically show flat, elevated lesions with an undulating surface, and "choroidal excavation" is rarely observed. The typical MRI appearance includes isointense or slightly hyperintense signals on T1WI, isointense or hypointense signals on T2WI, and less prominent enhancement compared to melanoma. A history of systemic malignancy, most commonly lung or breast cancer, is often reported.
Melanocytoma
This is a benign melanocytic tumor. Melanocytomas of the optic disc are generally small, located on one side of the optic disc, and appear as deeply pigmented black lesions with slight surface elevation. They typically exhibit no significant growth tendency. Melanocytomas located in the iris, ciliary body, or choroid can be larger and may show progressive growth. Their appearance and clinical presentation can resemble melanoma, making differentiation challenging, with histopathological diagnosis being the key determinant.
Treatment
Treatment approaches depend primarily on tumor size, location, and associated characteristics. For small to medium-sized UM, eye-preserving treatments such as plaque brachytherapy, transpupillary thermotherapy, particle beam therapy, or local resection are options. For large UM, treatments may include particle beam therapy, stereotactic radiotherapy, or enucleation. With advancements in technology, enucleation is no longer the first-line treatment for UM. However, in cases where the tumor continues to progress despite eye-preserving therapies, presents with optic nerve invasion, or leads to secondary glaucoma, enucleation is still necessary. For UM cases with orbital extension, orbital exenteration is required.
There are no specific therapeutic options for distant metastases. Available approaches include immunotherapy, chemotherapy, and targeted therapies.