Retinoblastoma (RB) is the most common intraocular malignant tumor in infants and young children, with an incidence rate of 1:16,000 to 1:18,000 in neonates. Approximately 90% of cases occur before the age of 3, with a familial inheritance tendency.
Genetics and Pathogenesis
The development of RB is influenced by genetic, epigenetic, and environmental factors. The primary cause is biallelic mutation or inactivation of the RB1 gene. In some cases without RB1 gene mutations, MYCN gene amplification is a major pathogenic factor. Epigenetic abnormalities, such as conformational changes in the long non-coding RNA GAU1, may also contribute to RB development and progression. Additionally, factors such as radiation exposure, advanced parental age, maternal HPV infection, and in vitro fertilization could promote the occurrence of RB.
Based on the timing and mechanism of RB1 mutation, RB can be categorized into four genetic types:
- Familial Inheritable Type: Patients inherit a mutated RB1 gene from an affected parent.
- Isolated Inheritable Type: No family history is present, and RB1 mutations occur in the zygote.
- Mosaic Type: RB1 mutations occur during the embryonic phase. If the mutation affects germ cells, it is inheritable; generally, it affects only one eye.
- Non-Heritable Type: Caused by somatic mutations in the RB1 gene, presenting with unilateral involvement, often with a single focal lesion.
The former two types tend to manifest early, follow an autosomal dominant inheritance pattern, affect both eyes, present with multifocal lesions, and have a higher risk of secondary primary tumors in other locations.
Clinical Manifestations
RB predominantly occurs in infants and young children and is not easily detected in its early stages. Leukocoria, also known as "cat's eye reflex," is the most typical symptom, observed in approximately 70% of patients at initial diagnosis. Tumor involvement of the macula may cause significant vision loss, often accompanied by sensory strabismus, which is seen in 10% of cases. Disease progression may lead to secondary glaucoma due to tumor cells blocking the anterior chamber, hyphema caused by the rupture of neovascular structures on the tumor or iris, or aseptic orbital cellulitis resulting from tumor necrosis. Symptoms such as eye redness and pain may also develop. Patients with trilateral RB (bilateral RB with an independent intracranial tumor) may exhibit signs such as headache, vomiting, fever, and seizures.

Figure 1 Leukocoria in a child with RB
The left pupil is dilated, with a diameter of approximately 5 mm. The pupillary light reflex is sluggish, and a central white reflex is visible.
Fundoscopy may reveal one or more yellowish-white solid elevated retinal masses. These masses may project into the vitreous humor or grow flat along the choroid, exhibiting various growth patterns:
- Exophytic Type: Tumor growth occurs from the outer nuclear layer of the retina into the subretinal space. Scattered or isolated poorly defined white lesions may be observed.
- Endophytic Type: Tumor growth occurs inward from the inner nuclear layer of the retina into the vitreous cavity. It appears as a flat, transparent, or pale mass with dilated and hemorrhagic retinal vessels on the surface.
- Mixed Type: Combines features of both the exophytic and endophytic growth patterns, commonly found in advanced RB.
- Cavitary Type: Formation of pseudocyst-like grayish-transparent cavities within the tumor, often seen in tumor remnants after volume-reducing treatment.
- Diffuse Infiltrating Type: Tumor cells infiltrate the retina and grow diffusely in a horizontal direction, without significant calcification.
- Diffuse Anterior RB Type: Characterized by tumor cell infiltration in the anterior chamber without retinal or vitreous involvement, or limited to lesions near the ora serrata with frequent vitreous seeding.
-
Diagnosis
Diagnosis primarily depends on the age of onset, family history, clinical signs, and fundoscopy findings, supplemented by imaging techniques such as ocular ultrasound, CT, and MRI. In most cases, a definitive diagnosis can be made. Peripheral blood genetic testing may assist in diagnosis for atypical cases. Intraocular biopsy is generally not advocated.
Ocular ultrasound may reveal echogenic masses of variable intensity in the vitreous cavity. Calcifications, reflected as highly echogenic shadowing, are present in 60% to 80% of cases.
CT Scan can identify calcifications and assess the extent of orbital or intracranial invasion, as well as the presence of pinealoblastoma.
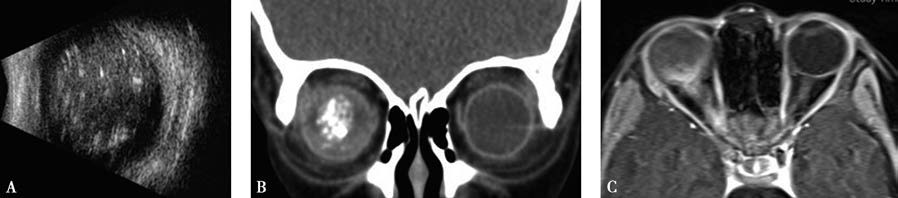
Figure 2 Imaging findings in a child with RB
A. Ocular ultrasound shows an echogenic mass with variable intensity in the right vitreous cavity, accompanied by calcifications.
B. CT reveals calcified foci within the right intraocular tumor.
C. MRI shows thickening and enhancement of the right optic nerve.
MRI offers higher resolution for soft tissue contrast and is currently the most sensitive imaging technique for evaluating orbital or extraocular extension of RB.
Differential Diagnosis
RB needs to be differentiated from other ocular conditions that may cause leukocoria:
Coats Disease (Exudative Retinopathy)
This is common among young males, typically presents unilaterally. Fundus features include abnormal retinal vessel dilation, large yellowish-white exudates under and within the retina, and cholesterol crystals. Exudative retinal detachment may be present, but calcification is rare.
Persistent Hyperplastic Primary Vitreous (PHPV)
This is a congenital ocular abnormality present at birth, caused by the failure of the embryonic primary vitreous to regress. It is usually unilateral, affects full-term infants, and presents as a fibrous vascular membrane behind the lens, causing leukocoria. Associated findings include microphthalmia, shallow anterior chambers, and smaller lenses.
Retinopathy of Prematurity (ROP)
This affects premature, low-birth-weight infants with a history of exposure to high concentrations of oxygen. Characterized by ischemia and hypoxia due to peripheral retinal vascular underdevelopment, ROP typically presents bilaterally and progresses to proliferative changes, tractional retinal detachment, and leukocoria in severe cases.
Endophthalmitis
In children, endophthalmitis mainly occurs after trauma. Infection by microbial pathogens involves the vitreous body, ciliary body, retina, and choroid. Vitreous abscesses may appear as yellowish reflexes through the pupil, resembling RB, but a history of ocular trauma and microbiological analysis of intraocular exudates confirm the diagnosis.
Treatment
Treatment options mainly include chemotherapy, laser therapy, cryotherapy, radiotherapy, and surgical interventions. For intraocular RB, classified into stages A, B, C, D, and E, only stage A and some stage B cases can be controlled with laser or cryotherapy. Most patients require a combination of chemotherapy and local treatments to preserve the eye. In stage E cases, especially those with clinical high-risk factors or orbital invasion, ensuring life safety often necessitates enucleation or, in some cases, orbital exenteration.
Chemotherapy
Chemotherapy can be categorized into intravenous chemotherapy and arterial chemotherapy based on the delivery route. Intravenous chemotherapy serves as the primary eye-preserving treatment for bilateral RB cases. It is also used for tumor volume reduction and as adjuvant therapy for advanced cases. Arterial interventional chemotherapy is currently the primary eye-preserving treatment for unilateral RB and significantly improves eye-preservation rates in advanced intraocular disease compared to intravenous chemotherapy.
Laser Therapy
This is suitable for tumors that are small, located in the posterior pole, and confined to the retina. It can be employed as a first-line treatment in stage A and stage B cases where the macula and optic disc are not involved, or as an adjuvant therapy following chemotherapy for tumor volume reduction.
Cryotherapy
This is best suited for RB located in the anterior regions of the equator. Liquid carbon dioxide is the most commonly used cryogen, capable of reaching temperatures as low as -80°C, leading to the formation of ice crystals within tumor and endothelial cells, thereby destroying the tumor cells.
Intravitreal Chemotherapy Injection
This is suitable for cases with vitreous seeding of tumor cells or subretinal seeding.
Vitrectomy with Tumor Excision
This is used selectively under strict indications and is not considered a first-line treatment. For bilateral RB cases where one eye has already been enucleated and the tumor in the remaining eye cannot be controlled with other eye-preserving methods, vitrectomy with tumor excision can be performed under melphalan perfusion to attempt to preserve the eye.
Enucleation
This is indicated for stage E cases, especially those with clinical high-risk factors, or when tumors show no response to or progression despite comprehensive treatment. During surgery, it is critical to remove as much of the optic nerve as possible to ensure adequate margins.
Orbital Exenteration
This is indicated when the tumor tissue has breached the globe and grown into the orbit or when there is optic nerve canal enlargement. Postoperative treatment typically combines radiotherapy and chemotherapy, although the prognosis is significantly worse than for intraocular-stage disease.