Adenoid cystic carcinoma of the lacrimal gland is the most common malignant epithelial tumor of the lacrimal gland.
Clinical Presentation
The onset of the disease exhibits a bimodal age distribution, with a major peak around 40 years of age and a minor peak in adolescence. The disease progression is relatively rapid, predominantly manifesting as proptosis or displacement of the eyeball. Patients may experience restricted eye movement and diplopia. Perineural invasion is a hallmark of adenoid cystic carcinoma of the lacrimal gland, often resulting in significant pain. CT scans reveal an isodense mass in the superotemporal orbit, with ill-defined margins showing creeping growth along the orbital walls toward the orbital apex and areas of moth-eaten bone destruction. On MRI, the tumor shows isointense signals on T1-weighted imaging (T1WI) and inhomogeneous signals on T2-weighted imaging (T2WI), with inhomogeneous enhancement after contrast administration. Histological subtypes include cribriform, tubular, and solid patterns, with the solid subtype associated with the poorest prognosis.
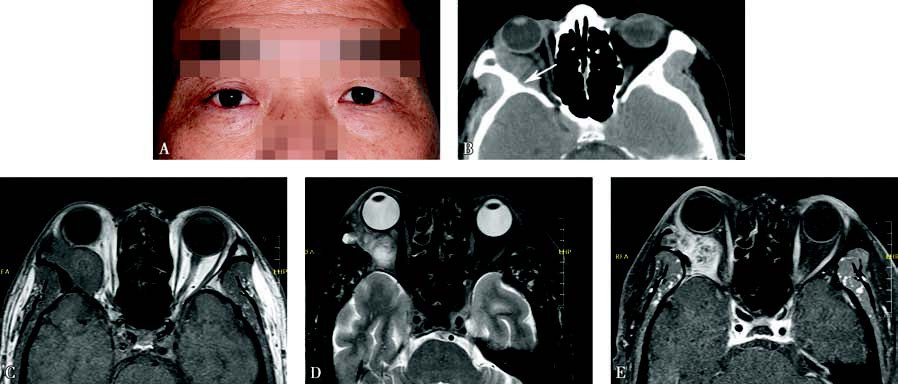
Figure 1 Appearance and imaging of adenoid cystic carcinoma of the lacrimal gland
A. A photograph of a patient with adenoid cystic carcinoma of the right lacrimal gland, showing proptosis of the right eye.
B. Axial CT imaging demonstrates a hyperdense mass in the extraconal space posterior to the globe, extending along the orbital walls toward the orbital apex and associated with bone destruction (white arrow).
C. MRI T1-weighted imaging shows an isointense signal from the tumor.
D. MRI T2-weighted imaging with fat suppression reveals inhomogeneous tumor signals.
E. Contrast-enhanced T1-weighted imaging demonstrates inhomogeneous enhancement of the tumor.
Treatment
The primary treatment involves extended local resection, followed by postoperative radiotherapy. Patients with systemic metastasis are treated with chemotherapy or combined targeted therapy.