Conjunctival melanoma (CM) originates from melanocytes in the basal layer of the conjunctival epithelium, accounting for 2%–7% of ocular melanomas. Among these, 65%–74% arise from malignant transformation of primary acquired melanosis (PAM), while the remainder originate from malignant transformation of conjunctival nevi or develop as de novo lesions.
PAM is a term that encompasses a group of non-nevogenic pigmented conjunctival epithelial lesions with variable pathological and histological features, accounting for 11% of conjunctival tumors. The classification of PAM lesions is based on the degree of melanocytic atypia. When atypical melanocytes involve the full thickness of the epithelium, the lesion is classified as melanoma in situ. PAM is more commonly seen in middle-aged and older women, with an unknown etiology. Lesions are most often located on the bulbar conjunctiva and may affect appearance. Flat and quiescent lesions usually present no symptoms. If the lesion becomes elevated, increases significantly in size, exhibits ulceration or bleeding, the possibility of malignant transformation should be considered.
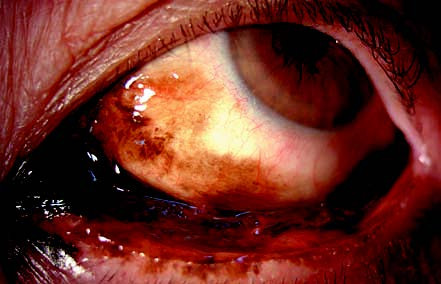
Figure 1 Primary acquired melanosis in the left eye
The lesion appears blackish-brown, diffusely involving the conjunctival fornix, tarsal conjunctiva, medial canthal skin, and parts of the bulbar conjunctiva. Pathological findings indicate mild to moderate atypia.
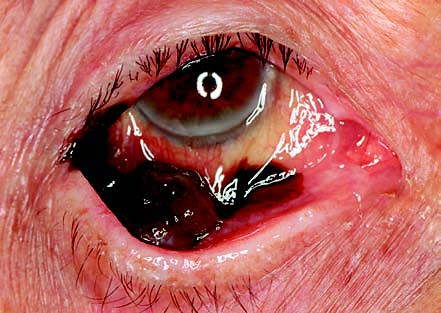
Figure 2 Conjunctival melanoma in the right eye
The lesion is located in the inferotemporal conjunctival fornix, extending to the surrounding tarsal and bulbar conjunctiva and parts of the eyelid margin. Prominent feeder vessels are observed, with indistinct lesion margins. The tumor is friable and bleeds easily upon contact.
Most CM patients seek medical attention after noticing an elevated lesion on the surface of the conjunctiva, foreign body sensations, or pain. The lesion may grow rapidly over a short period and tends to ulcerate and bleed. CM is most commonly found on the bulbar conjunctiva, but it can also occur on the tarsal conjunctiva and caruncle or invade the cornea. The tumor typically grows in a nodular fashion, though diffuse growth may occur in some cases. It is often richly vascularized, and the pigmentation of the tumor can vary in intensity. CM may invade the eyelid, orbit, lacrimal ducts, intraocular structures, and sinuses, and it can metastasize to regional lymph nodes or distant organs such as the brain, liver, lungs, and bones. Histologically, CM is characterized by varying combinations of atypical spindle cells, pleomorphic cells, and epithelioid cells.
Treatment
For lesions suspected to be CM, timely surgical treatment is necessary. Isolated lesions are treated with no-touch complete wide excision. Diffuse or multifocal lesions may require map biopsies or multiple site excisions, with an effort to preserve the eyeball. Cryotherapy and chemotherapy during surgery are important to reduce recurrence. CM carries a high risk of metastasis; in cases of regional spread, radical lymph node dissection should be performed. For patients with distant metastases, chemotherapy and targeted therapy may be implemented, though the overall prognosis remains poor.