Orbital blowout fracture occurs when external force is applied to the eye, causing a sudden increase in orbital pressure. The impact is transmitted to the orbital soft tissues, leading to fractures in the thin orbital walls. This results in herniation or entrapment of orbital soft tissues, often presenting with enophthalmos and restricted ocular motility.
Clinical Manifestations
Fractures of the orbital floor or medial wall are the most commonly observed types. The clinical symptoms and signs vary greatly depending on the location, extent, and configuration of the fracture, as well as the degree of soft tissue herniation.
In the early stages following trauma, swelling and hemorrhage of orbital soft tissues, as well as orbital emphysema associated with the fracture, increase orbital pressure. This, along with paralysis of the extraocular muscles, often leads to symptoms such as eyelid swelling and congestion, proptosis with restricted movement, bulbar conjunctival hemorrhage and edema, and in severe cases, prolapse of the conjunctiva beyond the palpebral fissure.
One to two weeks after the trauma, orbital bleeding and edema gradually resolve. Depending on the location and extent of the fracture, varying degrees of enophthalmos may develop. Extraocular muscle displacement, entrapment, or fibrosis leads to ocular misalignment, restricted eye movement, and diplopia. Enophthalmos and restricted ocular motility are the most common clinical manifestations of orbital blowout fractures.
Additionally, fractures involving the orbital floor are often associated with injuries to the infraorbital nerve, causing sensory deficits. Damage to the nasal cavity or paranasal sinuses may result in epistaxis or nasal bone fractures.
CT scanning serves as the standard diagnostic modality for orbital blowout fractures. Early imaging findings include swelling and hemorrhage of orbital soft tissues, orbital emphysema, bleeding into the paranasal sinuses, and orbital wall fractures. In later stages, imaging may reveal orbital wall fractures, orbital cavity expansion, extraocular muscle displacement and thickening, and enophthalmos.
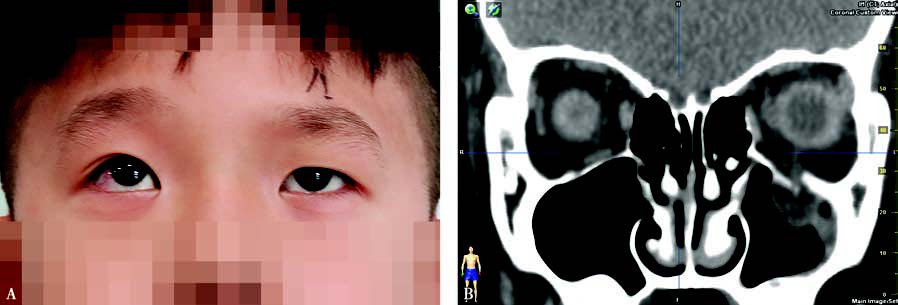
Figure 1 Left orbital fracture
A: Restricted upward gaze in the left eye. B: Coronal CT shows a left orbital floor fracture with herniation and entrapment of the inferior rectus muscle, involving the infraorbital nerve.
Treatment
Early management often focuses on symptomatic relief and reduction of orbital swelling. Localized cold compresses are utilized, and nose blowing is discouraged to prevent exacerbation of orbital emphysema. For patients with elevated orbital pressure, dehydration agents may be used. Antibiotics are administered in suspected cases of infection. Any cause of visual impairment is meticulously investigated and addressed. Symptoms in the nasal cavity and maxillofacial region require appropriate interventions.
Surgical treatment can be categorized into two approaches:
Urgent Surgery
This is recommended for cases involving entrapment of the extraocular muscles in the fracture line (commonly observed in pediatric patients, characterized by inability to move the eye past the midline). In such cases, early intervention is necessary to release the entrapped extraocular muscle during surgery.
Elective Surgery
This is typically performed 3 to 4 weeks after the injury. Absolute indications for surgery include restricted ocular motility and persistent diplopia, while relative indications include enophthalmos greater than 2 mm that affects facial appearance. The surgical approach involves repositioning herniated orbital soft tissues and using implantable materials to reconstruct the fractured orbital wall. Postoperative eye movement rehabilitation exercises are often required during the recovery period.