Orbital arteriovenous malformation is a high-flow congenital vascular anomaly of the orbit. It is characterized by blood shunting directly from supplying arteries through an abnormal vascular network (nidus) into the veins, bypassing the normal capillary bed. This condition can occur in various locations within or around the orbit.
Clinical Manifestations
Although orbital arteriovenous malformations are congenital, only a small proportion present visible defects in infancy or early childhood. Most patients develop symptoms after puberty, with unilateral cases being more common. Lesions located within the orbit are primarily characterized by painless proptosis, often accompanied by eyelid or conjunctival edema. If the optic nerve is affected, visual acuity and visual fields may be impaired. Lesions in periocular regions such as the eyelid can present as poorly defined soft tissue masses. The overlying skin may appear normal or exhibit redness, with increased surface temperature. Palpable pulsation or a thrill may also be noted.
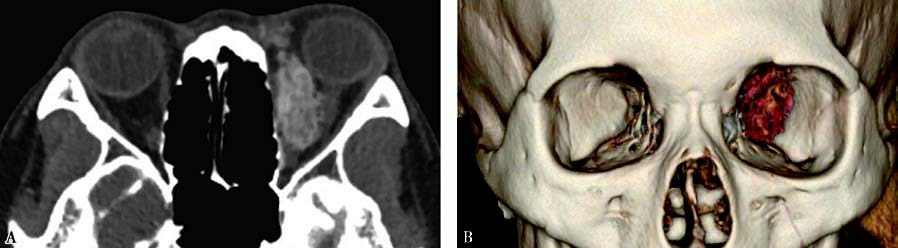
Figure 1 CT imaging of left orbital arteriovenous malformation
A. Contrast-enhanced CT image showing a poorly defined lesion with mixed density in the left orbit.
B. Three-dimensional reconstruction revealing an abnormal vascular mass along the medial orbital wall.
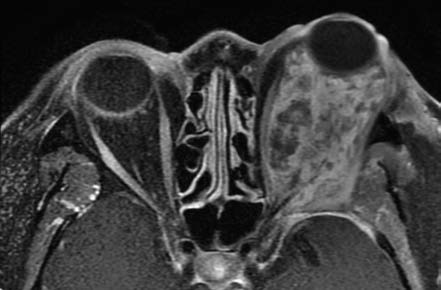
Figure 2 MRI imaging of left orbital arteriovenous malformation
Characteristic flow voids are observed within the lesion.
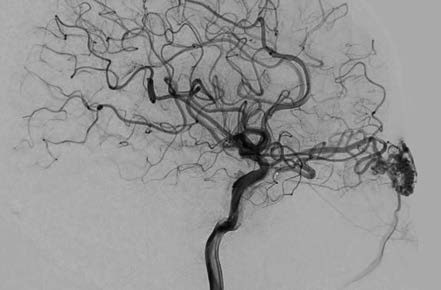
Figure 3 DSA imaging of orbital arteriovenous malformation
The feeding artery, vascular nidus, and draining vein are clearly visualized on angiography.
On CT imaging, orbital arteriovenous malformations often appear as poorly defined lesions with mixed-density signals, including hyperdense punctate or linear vascular structures. Some lesions may show hyperdense calcifications and hypodense areas of softening. Contrast-enhanced CT imaging often reveals worm-like enhanced clusters. MRI demonstrates the extent of the lesion and its anatomical relationships with great clarity. Both T1- and T2-weighted images exhibit characteristic flow voids, appearing as serpentine or globular low-signal areas within the lesion, surrounded by low signals from the feeding arteries and draining veins. Digital subtraction angiography (DSA) serves as the "gold standard" for diagnosing orbital arteriovenous malformations, providing detailed visualization of the feeding arteries, nidus, and draining veins.
Treatment
Due to the formation of arteriovenous shunts bypassing the normal capillary network, orbital arteriovenous malformations carry a risk of hemorrhage. The treatment goals are to reduce bleeding risk and eliminate the lesion. Primary treatment options include surgical excision, interventional therapy, and radiotherapy. Among these, transcatheter embolization with sclerotherapy involves minimal trauma and lower bleeding risk, making it a commonly used clinical approach.