Orbital cavernous venous malformation is the most common benign lesion within the orbit. It is characterized by abnormal vascular cavernous spaces with proliferation of vessels and stroma. This condition can occur in any location within the orbit.
Clinical Manifestations
Orbital cavernous venous malformations typically become symptomatic after young adulthood, with no gender predilection. The primary presentation is slow-onset proptosis, usually without subjective symptoms. Since many lesions occur within the muscle cone, early clinical manifestations include axial proptosis. Compression of the posterior pole of the globe may lead to retinal edema and dilated, tortuous veins, as well as visual changes due to refractive errors. Lesions originating in the orbital apex can compress the optic nerve, leading to early visual decline. Because these small lesions may not cause proptosis, they are often misdiagnosed clinically as refractive errors or optic neuritis.

Figure 1 CT imaging of a left orbital cavernous venous malformation
The lesion is well-defined, homogeneous in density, and compresses the optic nerve.

Figure 2 CT imaging of a right orbital cavernous venous malformation
A triangular hypodense area of orbital fat is visible at the orbital apex.
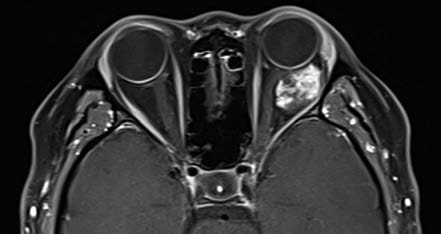
Figure 3 MRI imaging of a left orbital cavernous venous malformation
Progressive enhancement with early patchy enhancement.
On CT imaging, cavernous venous malformations typically appear well-demarcated and homogeneous in density. Signs such as optic nerve compression, displacement, and orbital cavity enlargement can be observed. CT imaging can also assess the degree of lesion adhesion. When fat is present at the posterior margin of the lesion, a triangular area of hypodense orbital fat is visible at the orbital apex on CT, suggesting minimal adhesion to surrounding tissues. Cavernous venous malformations without this hypodense orbital fat feature often exhibit significant adhesion. MRI findings show iso-intensity on T1-weighted images and hyperintensity on T2-weighted images. The hallmark of dynamic contrast-enhanced imaging is progressive enhancement, where small areas display early patchy enhancement that gradually becomes diffusely and homogeneously enhanced over time.
Treatment
Orbital cavernous venous malformations exhibit slow growth. If the lesion is small and asymptomatic, close clinical monitoring is appropriate. For lesions associated with significant clinical symptoms or if the patient desires treatment, surgical excision is an option. Preoperative imaging allows precise localization of the lesion and determines the optimal surgical approach.