Vertical strabismus is generally diagnosed based on the position of the elevated eye. The condition can have various causes. Congenital cases may be due to anatomical abnormalities (such as abnormal attachment points of extraocular muscles or absence of muscles) or neuromuscular paralysis. Acquired cases can result from closed head trauma, orbital wall fractures, orbital tumors, brainstem lesions, or systemic diseases. Vertical strabismus is almost always non-commutative. Its examination, diagnosis, and treatment are more complex compared to horizontal strabismus.
Superior Oblique Muscle Palsy
Superior oblique muscle palsy (SOP) is the most common form of vertical and torsional extraocular muscle paralysis. The etiology can be congenital, stemming from anatomical abnormalities, nuclear defects, or deficits in the motor components of the fourth cranial nerve. Acquired cases are often caused by head trauma but may also result from vascular abnormalities in the central nervous system or diabetes.
Congenital Superior Oblique Muscle Palsy (CSOP)
Diagnosis
Congenital superior oblique muscle palsy typically presents as hypertropia of the affected eye. In bilateral cases, alternating hypertropia occurs: the left eye appears hypertropic during right gaze and vice versa. In cases of asymmetry between the two eyes, incomplete palsy in the less-affected eye should be suspected. When both eyes are involved, vertical deviation in primary gaze is usually minimal. The head-tilt test is positive, with significant hypertropia or upward deviation of the affected eye when the head is tilted toward the elevated eye. In terms of eye movements, the affected eye experiences lag in nasal downward movement (due to reduced superior oblique function) and may show hyperfunction during upward nasal movement (due to inferior oblique overaction), while monocular movements can appear normal. Fundus photography often displays excyclotorsion.
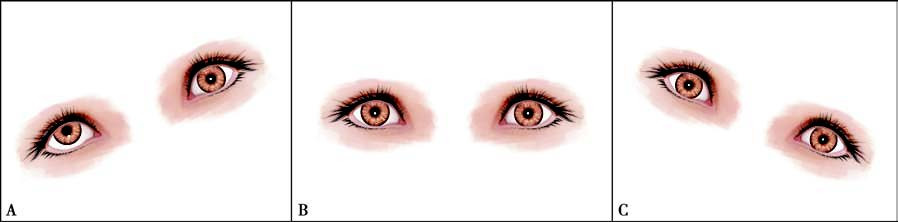
Figure 1 Positive head-tilt test in right eye congenital superior oblique palsy
A. Significant hypertropia of the right eye when the head is tilted to the right.
B. Slight hypertropia of the right eye in the primary position.
C. The right eye returns to a normal position when the head is tilted to the left.
Unilateral congenital superior oblique palsy may exhibit a characteristic compensatory head posture, with the head tilted toward the lower eye, the face turned toward the side of the healthy eye, and the chin tucked inward. Facial asymmetry is common in such cases. Amblyopia is rarely associated. Decompensated cases can present with diplopia.
Treatment
Surgical intervention is the primary approach. For small-angle strabismus or residual minor deviations after surgery, prismatic correction can be employed. Early surgery is recommended when objective examinations provide reliable results, as this can help restore binocular vision and reduce facial or skeletal development abnormalities. Surgical planning primarily focuses on weakening overacting muscles, such as weakening the inferior oblique muscle of the affected eye and/or the inferior rectus muscle of the contralateral eye. Strengthening the underperforming superior oblique muscle of the affected eye, such as through superior oblique tucking, is also an option, though weakening procedures typically yield more reliable outcomes.
Acquired Superior Oblique Muscle Palsy (ASOP)
Diagnosis
Acquired superior oblique muscle palsy is characterized by a sudden onset of diplopia. Although it may present in adulthood, some cases could involve decompensated congenital palsy. Reviewing old photographs is important in distinguishing congenital from acquired cases. Strabismus angle measurements and diplopia assessments in diagnostic eye positions, along with the Parks three-step test, can identify the affected eye and muscle. Eye movement tests, particularly versions, may reveal varied limitations in nasal downward movement. Overaction of the ipsilateral inferior oblique muscle is generally not prominent. Compensatory head posture is present but less pronounced compared to congenital cases.
Treatment:
Management should focus on identifying and addressing the underlying cause. For cases where no clear etiology is established following multiple examinations, symptomatic treatment is initiated. For cases with clear causality and stable strabismus persisting for six months, surgical correction is performed to realign the eyes in primary and inferior gaze positions and restore binocular vision. Prismatic correction can effectively address small-angle vertical deviations (typically <10Δ) but is less helpful for torsional misalignments.
Double Elevator Palsy
Double elevator palsy, also known as monocular elevation deficiency, describes paralysis of both the superior rectus and inferior oblique muscles in one eye.
Diagnosis
Both nasal and temporal upward movements of the affected eye are restricted, leading to hypertropia of the opposing eye in primary gaze. The alignment of the affected eye becomes even lower in upward gaze. Associated amblyopia may be present. Patients often adopt a compensatory chin elevation posture. Ptosis of the affected eye is common, though 50% of cases involve pseudoptosis. About one-third of patients may exhibit Marcus Gunn jaw-winking syndrome.
Treatment
Surgical intervention is the primary treatment. When inferior rectus restriction is identified, inferior rectus recession is performed. In the absence of restriction, horizontal rectus muscle transposition is performed, such as the Knapp procedure, where the medial and lateral rectus muscles are repositioned to the superior rectus insertion.
A- and V-Pattern Strabismus
A- and V-pattern strabismus is a subtype of horizontal strabismus in which the angle of deviation remains largely constant in the horizontal gaze but changes significantly in different vertical gaze positions. It can be understood as a non-commutative horizontal strabismus during vertical gaze, forming patterns resembling the letters "A" or "V." The open ends of the letters indicate weaker convergence or stronger divergence, while the apex of the letters indicates stronger convergence or weaker divergence. About 15%–25% of strabismus cases are associated with A- and V-patterns. In V-pattern exotropia, the angle of deviation is greater in upward gaze than in downward gaze. In A-pattern exotropia, the angle is greater in downward gaze than in upward gaze. In V-pattern esotropia, the angle is smaller in upward gaze than in downward gaze. In A-pattern esotropia, the angle is smaller in downward gaze than in upward gaze.
Diagnosis
Horizontal deviations are measured while the patient looks 25° upward and 25° downward at a distance. In V-pattern strabismus, the difference in the deviation angle between upward and downward gaze is ≥15Δ. In A-pattern strabismus, the difference is ≥10Δ. Eye movement examinations are essential to determine whether there is abnormal oblique muscle function. A-pattern strabismus is frequently associated with overaction of the superior oblique muscle, whereas V-pattern strabismus is often associated with overaction of the inferior oblique muscle.
Treatment:
For V-pattern strabismus, in cases where overaction of the inferior oblique muscle is present, inferior oblique weakening procedures are performed, regardless of the degree of overaction, before correcting the horizontal strabismus. For cases without inferior oblique overaction, the vertical transposition of horizontal rectus muscles is performed during horizontal strabismus correction.
For A-pattern strabismus, if stereopsis is present, superior oblique weakening procedures are contraindicated, and the A-pattern is corrected by vertically transposing the horizontal rectus muscles. For cases without stereopsis and obvious superior oblique muscle overaction, superior oblique weakening procedures are typically performed first, followed by horizontal strabismus correction. If superior oblique overaction is mild or absent, vertical transposition of the horizontal rectus muscles is used instead.
For correction using horizontal muscle transposition in A- and V-pattern strabismus, the medial rectus muscles are transposed toward the apex of the A or V pattern, while the lateral rectus muscles are transposed toward the open end of the letters.