Esotropia refers to an inward deviation of the visual axes, and it can be categorized into comitant esotropia and noncomitant esotropia. Comitant esotropia is the most common form of strabismus in infants and young children, and it can be further divided into non-accommodative and accommodative esotropia. Infantile esotropia is a specific type of non-accommodative esotropia, typically presenting within the first six months of life, and is also referred to as congenital esotropia.
The primary goal in the treatment of esotropia is the restoration of binocular vision. Childhood esotropia significantly impacts binocular vision and can easily lead to amblyopia. Upon diagnosis, treatment should begin as soon as possible, initially focusing on addressing the perceptual deficits caused by esotropia, including suppression and amblyopia. Once the visual acuity of both eyes is nearly balanced, esotropia is corrected using non-surgical or surgical interventions. Early surgical intervention is often recommended if esotropia negatively affects a child’s psychological development or social interactions. Adults with acquired esotropia are initially treated conservatively while actively investigating the underlying causes. If the cause is identified and the condition stabilizes for six months, surgical correction may be performed.
Several factors influence the choice of extraocular muscles for surgical correction. The deviation angle in the primary gaze position is a key consideration, along with the differences in deviation angles for distance and near vision. The medial rectus muscles are more effective in correcting near-angle esotropia, while the lateral rectus muscles are more effective for distance-angle esotropia. For patients with larger near esotropia, bilateral weakening procedures on the medial rectus muscles are typically performed, such as bilateral medial rectus recession. In cases where the deviation angles for near and distance vision are similar, combined procedures such as bilateral medial rectus weakening and lateral rectus muscle strengthening, such as lateral rectus resection, yield comparable results. It should be noted that no more than two rectus muscles should typically be operated on during a single intervention on one eye to avoid anterior segment ischemia. Surgical correction only serves as a mechanical adjustment of ocular alignment, while other factors, such as the intrinsic properties of the muscles, their relationships with surrounding tissues, and different neural inputs, significantly influence surgical outcomes. Achieving satisfactory results may require multiple procedures.
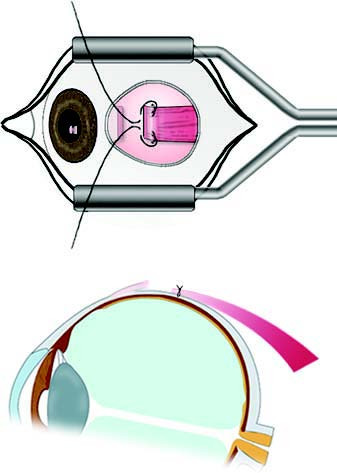
Figure 1 Medial rectus recession surgery
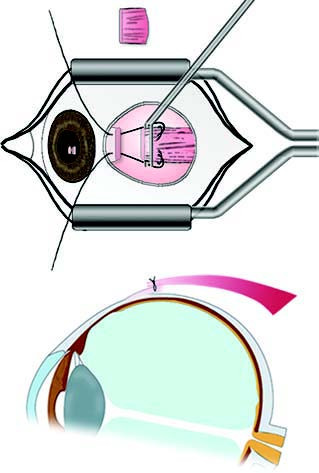
Figure 2 Medial rectus resection surgery
Congenital Esotropia (Infantile Esotropia)
Diagnosis
Key diagnostic features:
- Onset occurs within the first six months of life, typically without significant refractive errors.
- Frequent alternating fixation with minimal amblyopia, although unilateral esotropia can be associated with amblyopia.
- Large deviation angles are present.
- Pseudorestriction in abduction may occur, which can be excluded using the “doll’s head” maneuver.
- Accompanying conditions such as inferior oblique overaction, dissociated vertical deviation (DVD), and nystagmus may also be observed.
Treatment
Surgery is the primary form of treatment. In cases of unilateral amblyopia, amblyopia therapy is performed first. Surgical correction is undertaken once binocular vision is nearly balanced and alternating fixation is achieved, typically between 18 to 24 months of age.
If inferior oblique overaction or DVD is present, these should be taken into account during surgical planning, with inferior oblique transposition surgery used to address inferior oblique overaction and associated DVD.
Postoperative alignment leaving a residual microesotropia of less than 10 prism diopters is preferred to facilitate peripheral fusion and coarse stereopsis.
Accommodative Esotropia
Accommodative esotropia can result from two distinct or combined mechanisms: refractive accommodative esotropia caused by moderate-to-high hyperopia that requires increased accommodation to achieve a clear image, and high AC/A ratio accommodative esotropia, where a given amount of accommodation induces excessive convergence due to an abnormally high AC/A ratio.
Refractive Accommodative Esotropia
Diagnosis
Key diagnostic features:
- The average onset age is around two and a half years.
- Patients exhibit moderate-to-high hyperopic refractive errors.
- Cycloplegic refraction or appropriate corrective lenses can fully correct the strabismus.
- Unilateral esotropia may be associated with amblyopia, and ocular motility is typically unrestricted.
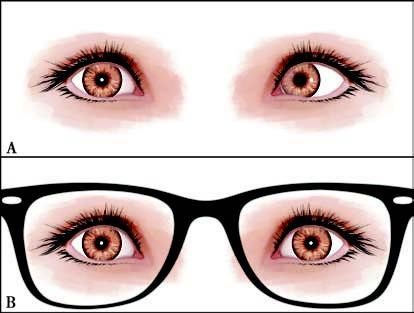
Figure 3 Refractive accommodative esotropia
A. Esotropia of the left eye without glasses.
B. Complete correction of esotropia following full hyperopic correction.
Treatment
Full hyperopic correction is prescribed using glasses. Amblyopia, if present, is treated appropriately.
Surgical correction is not suitable for this type of esotropia.
Refraction is reassessed annually, and glasses are adjusted according to changes in refractive error. Earlier reassessment may be performed if required.
When adjusting prescriptions, visual acuity and ocular alignment should remain normal. If mild exotropia occurs with glasses, the spherical power should be reduced slightly, aiming for orthophoria or a mild esophoria with glasses.
Partially Accommodative Esotropia
Diagnosis
Key diagnostic features:
- Patients exhibit moderate-to-high hyperopic refractive errors.
- Cycloplegic refraction or corrective lenses reduce the deviation angle but cannot fully correct it.

Figure 4 Partially accommodative esotropia
A. Esotropia of the left eye without glasses.
B. Partial correction of esotropia following full hyperopic correction.
Treatment
Initial treatment involves full hyperopic correction with glasses. Amblyopia, if present, is addressed.
If the esotropia is not fully corrected after wearing glasses for three to six months, surgical correction of the non-accommodative component is performed, while the accommodative component continues to be managed with glasses.
Refraction is reassessed every six months to one year, and glasses are adjusted according to changes in refractive error.
When adjusting prescriptions, the principles are the same as for refractive accommodative esotropia, aiming for normal visual acuity and ocular alignment.
High AC/A Ratio Accommodative Esotropia
Diagnosis
Key diagnostic features:
- High AC/A ratio accommodative esotropia is characterized by a greater deviation angle at near compared to distance (≥15△) and may present with orthophoria at distance. Hyperopic refractive errors are often present. This type of esotropia tends to resolve spontaneously after the age of 10.
Treatment
Conservative treatments include bifocal lenses with full hyperopic correction plus an additional +1.50 to +3.00D sphere, or the use of miotics to reduce accommodative convergence at near, addressing the excessive esotropia at near distances.
In appropriate cases, surgical intervention may be considered. Bilateral medial rectus recession is commonly performed, sometimes combined with posterior fixation sutures to minimize the impact on distance alignment.
Non-Accommodative Esotropia
Non-accommodative esotropia includes the following subtypes:
Basic Esotropia
Diagnosis
Key diagnostic features:
- Basic esotropia typically develops after six months of age and is not associated with significant accommodative factors.
- Unilateral esotropia may be accompanied by amblyopia.
- No significant hyperopic refractive errors are observed, and the deviation angles for both near and distance vision are similar.
Treatment
Surgical correction is the main form of treatment. Amblyopia therapy is performed first if present, and surgery is conducted after achieving near-balanced binocular visual acuity to restore ocular alignment.
Although most children with basic esotropia exhibit no systemic symptoms, central nervous system examinations should still be considered.
Acute Comitant Esotropia
Diagnosis
Key diagnostic features:
- Acute comitant esotropia has a sudden onset, often accompanied by diplopia.
- It typically occurs after the age of five and does not involve significant limitations in ocular motility.
Treatment
Neurological examination is essential to exclude intracranial pathology, given the sudden onset of diplopia.
In the early stages, botulinum toxin type A injections can temporarily paralyze the medial rectus muscles to restore balance between the medial and lateral rectus muscles, reducing or eliminating strabismus after repeated injections.
Prism glasses can also be used to align the visual axes and eliminate diplopia in the primary and reading gaze positions.
Once the condition stabilizes, prism glasses can continue to be used, or surgical correction may be performed. In acute comitant esotropia, larger surgical dosages are typically required compared to other forms of esotropia to minimize the risk of residual deviation and recurrence. Binocular vision may partially recover after alignment is restored.
Cyclic Esotropia
Diagnosis
Key diagnostic features:
- Cyclic esotropia typically manifests between the ages of three and four. The esotropia presents in a periodic pattern, often alternating every other day with a 48-hour cycle.
- On non-esotropic days, only mild phoria or esophoria may be present, but the condition can progress to constant esotropia over time.
- Amblyopia is uncommon in patients with cyclic esotropia. V-pattern strabismus is frequently observed. On non-esotropic days, patients may exhibit normal binocular single vision and good stereopsis.
Treatment
Refractive errors are corrected first. In some cases, cyclic esotropia resolves following hyperopic correction.
For those who do not respond to refractive correction, surgical alignment is performed, referencing the deviation angle observed on esotropic days when planning surgical dosage.
Sensory Esotropia
Diagnosis
Key diagnostic features:
- Sensory esotropia occurs when significant unilateral vision loss or impairment develops during childhood due to conditions such as cataract, corneal leukoma, retinal disorders, optic nerve atrophy, or ocular trauma.
Treatment
Treatment involves addressing the underlying cause, correcting refractive errors, and treating amblyopia caused by media opacities. It is crucial in infancy and early childhood to preserve normal and symmetrical neural input in both eyes.
If residual esotropia persists after resolving the underlying cause, surgical correction of ocular alignment is performed.
Consecutive Esotropia
Diagnosis
Key diagnostic features:
- Consecutive esotropia often develops as a secondary complication following surgical correction for exotropia.
Treatment
Alternating patching is used in the early stages. If esotropia persists for more than two weeks, cycloplegic refraction can guide the prescription of full hyperopic correction. High AC/A ratio cases may benefit from bifocal lenses.
If esotropia persists for over four weeks, prism glasses are prescribed to eliminate diplopia and prevent amblyopia, with the minimum prism strength needed to achieve these goals.
In cases where esotropia ≥10△ persists for six months or more, surgical correction is recommended. Various factors influence surgical planning, including the near and distance deviation angles, the initial surgical dosage, limitations in ocular motility, and the visual acuity of each eye. In most cases, the second surgery involves re-exploration and repositioning of the recessed muscle(s) from the previous procedure.
Noncomitant Esotropia
Noncomitant esotropia is often associated with abducens nerve palsy.
Diagnosis
Key diagnostic features:
- Abducens nerve palsy is the most common form of cranial nerve palsy affecting ocular motility. It is most often acquired and can result from intracranial pathology, trauma, or peripheral viral infections. In some cases, no clear cause can be identified, but risk factors such as hypertension or diabetes-related microvascular changes may be present.
- Patients typically exhibit a large-angle esotropia, with limitation or loss of abduction. In severe cases, the affected eye cannot abduct beyond the midline. Compensatory head posture may occur, with the face turned toward the side of the affected muscle.
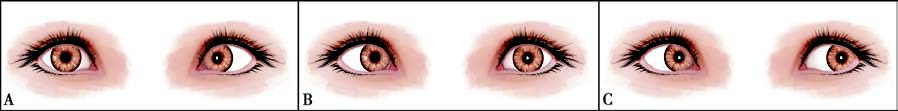
Figure 5 Right abducens nerve palsy
A. Limitation of right eye abduction.
B. Esotropia in primary gaze of the right eye.
C. Normal adduction of the right eye.
Treatment
Efforts are made to investigate the lesion causing the palsy to determine the underlying cause. Multidisciplinary consultation may be required in some cases.
For cases with a clear etiology, causative treatments are prioritized. Neurotrophic medications may be used to address nerve palsy.
Most cases recover spontaneously within approximately three months. For patients with a clear diagnosis and stable condition who still exhibit strabismus after six months, surgical correction of esotropia can be considered.
In cases of partial paralysis of the lateral rectus muscle, surgical options include weakening of the medial rectus muscle combined with strengthening of the lateral rectus muscle. For complete paralysis of the lateral rectus muscle, procedures such as weakening of the medial rectus muscle combined with vertical rectus muscle transposition can be performed.
Abducens nerve palsy is more commonly observed in adults. Adjustable sutures may improve the success rate of strabismus surgery in these cases. Preoperative assessment of the patient’s tolerance for adjustable sutures is required, and the potential discomfort of the procedure should be explained to the patient.
Injection of botulinum toxin type A into the medial rectus muscle may prevent or reduce muscle contracture without compromising blood supply from the ciliary circulation. This approach may serve as an alternative to medial rectus weakening surgery and can be repeated as needed.