Pathogenesis
With increasing age, the amplitude of accommodation gradually declines, resulting in difficulties with near work and related symptoms. This age-related physiological decline in accommodative ability is referred to as presbyopia. Regardless of an individual's refractive status, presbyopia eventually affects everyone.
The development of presbyopia is associated with a series of changes in the lens and the ciliary muscles. According to Helmholtz's theory, the lens thickens and increases in density with age, while its elasticity diminishes, leading to a reduced ability to change shape. Schachar's theory posits that the equatorial diameter of the lens increases with age, and the distance between the ciliary body and the lens equator decreases, reducing the effective contraction distance, and thereby lowering accommodative amplitude.
Clinical Manifestations
Symptoms
The appearance of presbyopic symptoms is directly related to age, typically beginning between 40 and 45 years old. Key symptoms include:
- Difficulty with near vision: Individuals with presbyopia gradually notice an inability to read small print at their usual comfortable working distance. They may need to hold books or newspapers farther away or tilt their head back to see clearly. Additionally, the required reading distance increases with age.
- Reduced ability to sustain near vision: To focus on near objects, individuals with presbyopia strain their accommodation. Near tasks often push their accommodative system to its limits, causing sustained contraction of the ciliary muscles, which in turn triggers overconvergence. Consequently, difficulty sustaining near vision may result in fluctuating vision, eye strain, tearing, and headaches—symptoms commonly associated with visual fatigue.
- Increased need for brighter illumination: In dim lighting, the pupils dilate, reducing depth of field, which makes near vision even more blurry. Adequate lighting, on the other hand, causes pupil constriction and increases depth of field while also enhancing text contrast, thus improving reading vision.
Factors Influencing Presbyopia
The onset and severity of presbyopia symptoms are influenced by several factors:
- Refractive status and correction methods: In uncorrected emmetropia, the far point is at optical infinity, while in myopia, the far point is closer to the eye. Presbyopia symptoms appear earlier in emmetropes than in myopes. Additionally, myopes who wear contact lenses, which rest directly on the cornea, tend to experience presbyopia symptoms earlier than when wearing glasses, as glasses sit 12–15 mm away from the cornea. Based on optical principles, the accommodative demand is higher when wearing contact lenses for near tasks compared to glasses. Conversely, hyperopes experience earlier symptoms when wearing glasses compared to contact lenses.
- Visual tasks: The accommodative demand is directly related to working distance and task precision. Those engaged in tasks requiring close, detailed work are more likely to experience presbyopia symptoms earlier than those performing tasks at greater distances.
- Physical characteristics: Taller individuals generally have longer arms, enabling them to hold reading materials farther away, thereby reducing the accommodative demand. As a result, taller individuals may exhibit presbyopia symptoms later than others.
- Geographic location: Epidemiological studies have shown that individuals living in equatorial regions tend to report presbyopic symptoms earlier than those in higher latitudes.
- Medications: Drugs that affect the ciliary muscles, such as insulin, anxiolytics, antidepressants, antipsychotics, antihistamines, antispasmodics, and diuretics, can lead to an earlier onset of presbyopia symptoms.
Diagnosis
The diagnosis of presbyopia is based on age, clinical symptoms, and the measurement of near addition. It is first necessary to perform standard objective and subjective refraction procedures to correct any underlying refractive error before measuring near addition. If the measured near addition is greater than zero, the presence of presbyopia is confirmed, and corrective measures are required. The process of measuring near addition involves two steps:
Trial Near Addition
This step involves determining the accommodative amplitude of the patient, either through direct measurement or by referencing the Donder’s table to find the expected accommodative amplitude for the patient’s age. The principle of “reserving half the accommodative amplitude” can then be applied to determine the trial near addition. An alternative method involves using the fused cross cylinder (FCC) test, which employs a Jackson Cross Cylinder (JCC) lens and FCC testing chart on a phoropter. This approach calculates the patient’s accommodative lag to estimate the appropriate trial near addition.
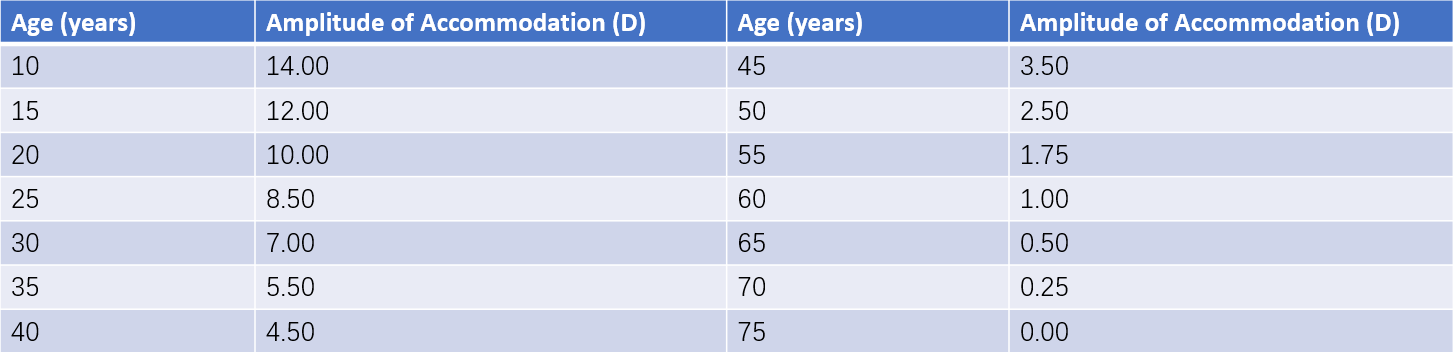
Table 1 Donder’s table of amplitude of accommodation
Final Near Addition
Using a phoropter and starting with the trial near addition, the negative relative accommodation (NRA) and positive relative accommodation (PRA) are measured. The average of the NRA and PRA values is added to the trial near addition to calculate the final near addition.
Correction
The goal of presbyopia correction is to use positive lenses to compensate for the physiological decline in accommodative ability, thereby addressing difficulties with near vision. Modern correction principles increasingly focus on providing patients with clear vision across far, intermediate, and near distances. With the advent of aging societies worldwide, research on restoring or reconstructing accommodative ability in the human eye has become a significant focus of future advancements in ophthalmology.
Correction with Eyeglasses
Eyeglasses for correcting presbyopia can be categorized into three types: single-vision lenses, bifocal lenses, and progressive additional lenses (PALs). Single-vision lenses are designed solely for near vision correction. Bifocal lenses combine two different dioptric powers into a single lens, addressing the needs for both distance and near vision. Progressive additional lenses are designed with a gradient of refractive power across the lens, structured into three zones from top to bottom: the distance vision zone, the transitional zone, and the near vision zone. The transitional zone connects the distance and near vision zones with a gradually changing curvature, providing clear intermediate vision and enabling seamless transitions between far, intermediate, and near distances. Externally, progressive lenses appear indistinguishable from regular single-vision lenses, as they lack visible dividing lines. In addition to eliminating the need for frequent removal and replacement for distance or near vision adjustments, these lenses also avoid drawing attention to aging, making them widely adopted as the first choice for presbyopia correction.

Figure 2 Progressive additional lens (PAL)
Correction with Contact Lenses
Contact lens correction for presbyopia includes two primary approaches: simultaneous vision designs and monovision designs. Simultaneous vision contact lenses are available in various designs, including segmented bifocal, concentric bifocal, ring-zone multifocal, and progressive multifocal lenses. Monovision involves correcting one eye (usually the dominant eye) for distance vision and the other for near vision. Using the principle of visual cortical preference for clear images, this approach suppresses the blurred image from the non-dominant eye.
Surgical Treatment
Surgical options for presbyopia fall into two categories. The first includes procedures specifically targeting presbyopia correction, such as corneal laser surgery or scleral expansion surgery. Scleral expansion aims to increase the space between the ciliary muscles and the equatorial area of the lens, enhancing the lens's ability to change shape and thereby addressing presbyopia. The second category involves combining presbyopia correction with cataract or lens replacement surgery, where multifocal intraocular lenses (MIOLs) or accommodative intraocular lenses (AIOLs) are implanted during cataract removal. These intraocular lenses enable patients to achieve clear vision for both far and near distances post-surgery.