Astigmatism is a refractive condition in which the refractive power of the eye varies between different meridians, preventing parallel light rays from focusing at a single point after passing through the eye.
Etiology and Pathogenesis
Astigmatism arises due to anatomical factors such as uneven curvature of the cornea and the lens across different meridians, or asymmetry in their alignment along the optical axis. These variations cause differences in the refractive power of the eye's optical system across the meridians. A certain degree of astigmatism can occur physiologically, and it is relatively rare for an eye to have absolutely no astigmatism.
Certain ocular diseases can also result in astigmatism. For example, keratoconus and corneal scars may cause irregular astigmatism that cannot be corrected with eyeglasses. External forces compressing the cornea, such as chalazion or ocular tumors, may alter corneal curvature and induce astigmatism. Early-stage cataracts may cause localized changes in the refractive index of the lens, leading to astigmatism. In cases of zonular fiber defects, lens dislocation and lens asymmetry relative to the optical axis can also lead to astigmatism. Furthermore, ophthalmic surgeries may result in surgically induced astigmatism. High myopia and procedures like retinal detachment surgery involving scleral buckling may cause retinal tilting, resulting in astigmatism.
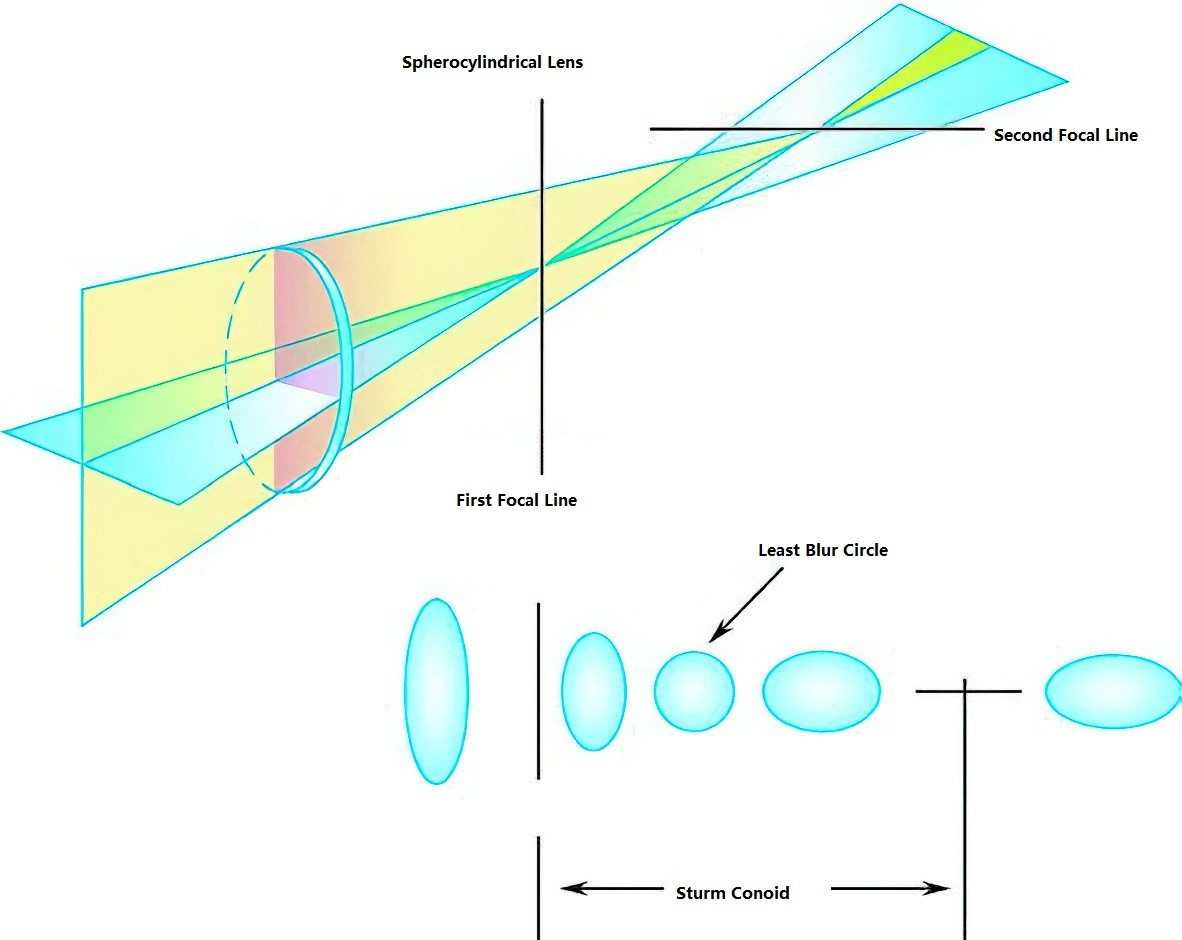
Figure 1 The Sturm conoid of astigmatism
For regular astigmatism, light rays passing through the refractive media of the eye do not converge at a single point but instead form a three-dimensional shape known as the Sturm conoid. Light rays passing through the meridian with the greatest refractive power converge earlier, forming a focal line located closer to the eye. Meanwhile, light rays passing through the meridian with the least refractive power converge later, forming a focal line farther from the eye. Between these two focal lines lies the least blur circle, a plane where the spread of light in all meridians is minimized.
Classification
Classification by Regularity
Astigmatism can be divided into regular astigmatism and irregular astigmatism.
Regular Astigmatism
The two principal meridians with the maximum and minimum refractive powers are perpendicular to each other. Along a given meridian, the refractive power at all points is uniform.
Irregular Astigmatism
The two principal meridians are not perpendicular, or the curvature along the same meridian varies irregularly.
Regular astigmatism can be further classified according to the orientation of the meridian with the greatest refractive power:
- With-the-Rule Astigmatism: The meridian with the greatest refractive power is oriented vertically (90° ± 30°). When corrected with a negative cylindrical lens, the axis of the cylinder is oriented horizontally (180°–30° or 150°–180°).
- Against-the-Rule Astigmatism: The meridian with the greatest refractive power is oriented horizontally (180°–30° or 150°–180°). When corrected with a negative cylindrical lens, the axis of the cylinder is vertical (90° ± 30°).
- Oblique Astigmatism: The meridian with the greatest refractive power is oriented obliquely (30°–60° or 120°–150°).
In children, tightened eyelids can exert pressure on the superior and inferior corneal surfaces, creating a shape similar to a horizontal positive cylindrical lens. This results in with-the-rule astigmatism, which is often balanced by against-the-rule astigmatism in the lens. In older adults, eyelid laxity makes against-the-rule astigmatism more common.
Classification by Focus Location Relative to the Retina
Regular astigmatism can also be classified based on how the focal lines of the two principal meridians relate to the retina:
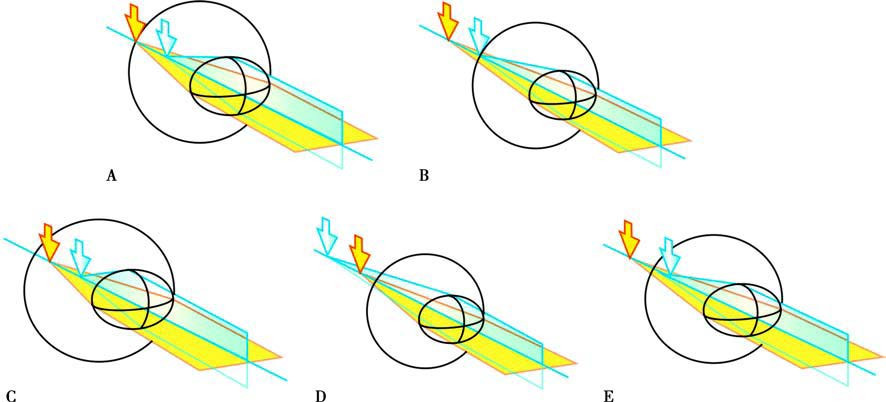
Figure 2 Five types of astigmatism
A. Simple Myopic Astigmatism
B. Simple Hyperopic Astigmatism
C. Compound Myopic Astigmatism
D. Compound Hyperopic Astigmatism
E. Mixed Astigmatism
Simple Myopic Astigmatism
One focal line is on the retina, while the other is in front of the retina.
Simple Hyperopic Astigmatism
One focal line is on the retina, while the other is behind the retina.
Compound Myopic Astigmatism
Both focal lines are in front of the retina.
Compound Hyperopic Astigmatism
Both focal lines are behind the retina.
Mixed Astigmatism
One focal line is in front of the retina, while the other is behind it.
When astigmatism is mild and the least blur circle is located on the retina, its impact on vision is minimal.
Classification by Source
Astigmatism can be classified based on its origin into corneal astigmatism and internal astigmatism:
Corneal Astigmatism
Astigmatism is caused by the anterior surface of the cornea.
Wearing rigid contact lenses can create a "tear lens" that improves the regularity of the optical surface, helping to correct irregular astigmatism originating from the anterior corneal surface.
Internal Astigmatism
Astigmatism arises from other parts of the eye, such as the posterior corneal surface, the lens, or the retina. Internal astigmatism cannot be corrected with rigid contact lenses.
Total astigmatism represents the vector sum of corneal and internal astigmatism.
Diagnosis
Symptoms
Uncorrected astigmatism prevents both distant and near objects from forming clear images on the retina, resulting in reduced visual acuity at all distances. Severe astigmatism during infancy and early childhood, if left uncorrected, can significantly impair visual development and lead to amblyopia. When the least blur circle coincides with the retina, the overall clarity of vision in astigmatic eyes may improve. However, when either the anterior or posterior focal line of the Sturm conoid aligns with the retina, the retinal image of the observed object may have sharper contour lines in a specific direction. To improve visual clarity, individuals with astigmatism may use accommodation to bring the least blur circle or one of the focal lines closer to the retina. Prolonged accommodation can lead to tension in the ciliary muscles, resulting in symptoms such as visual fatigue, fluctuating vision, image distortion, eye pain, and headaches.
The severity of visual fatigue does not necessarily correspond to the amount of astigmatism. Patients with relatively low amounts of astigmatism often report more subjective symptoms. In contrast, individuals with high levels of astigmatism or a Sturm conoid located far from the retina, to the extent that accommodation cannot improve clarity, may exhibit minimal symptoms of visual fatigue but show significant reductions in visual acuity.
In cases of simple myopic astigmatism or simple hyperopic astigmatism, patients may display a unique recognition pattern when tested with an "E" chart, distinguishing between horizontal or vertical contours of optotypes more clearly. For instance, patients may only be able to discern the direction of the optotype's openings. Some individuals may also exhibit habitual squinting. Oblique astigmatism can lead to head tilting to one side in an attempt to reduce image tilt, which, in young children, may develop into a condition resembling torticollis. Distinction from conditions like vertical strabismus or abnormalities of the sternocleidomastoid muscle is necessary in such cases. When astigmatism is corrected for the first time with glasses, patients may experience temporary image distortion and tilt due to the brain's adaptation to previously distorted images.
Examinations
Refraction Testing
Refraction results provide the degree and axis of total astigmatism in the eye, expressed in terms of cylindrical power and axis. Based on refraction results, the spherical equivalent (SE) can be calculated as spherical power + 1/2 cylindrical power. The spherical equivalent determines the location of the least blur circle, with larger spherical equivalents placing the least blur circle further from the retina.
Ciliary muscle contraction should produce uniform contraction forces in all directions, resulting in evenly distributed tension on the zonular fibers. In such cases, accommodation affects only the power of the spherical component in refraction testing. However, if the contraction forces of different parts of the ciliary muscle are uneven, the asymmetric tension on the lens can lead to changes in cylindrical power and axis. This phenomenon results in differences between refractive status at far and near distances, requiring separate refraction for distance and near vision.
Clock Dial Test
This subjective test can detect astigmatism. When both the anterior and posterior focal lines are located in front of the retina due to under-correction of myopia, patients viewing an astigmatic chart will perceive one direction as clearer and its perpendicular direction as blurrier. This occurs because the posterior focal line is closer to the retina, while the blurry direction corresponds to the anterior focal line, located further away from the retina.
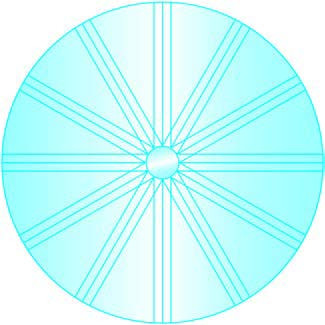
Figure 3 Clock dial
Corneal Topography
This test provides information about the shape and degree of corneal astigmatism. In cases of high astigmatism, corneal topography helps identify the primary source of the astigmatism.
Management
Unlike myopia and hyperopia, which are typically corrected with spherical lenses, astigmatism is generally corrected using cylindrical lenses. Combined myopia or hyperopia with astigmatism requires correction with sphero-cylindrical lenses. Correction methods include eyeglasses, contact lenses, or refractive surgery.
When high astigmatism is first corrected with eyeglasses, the significant difference in magnification between meridians can lead to severe image distortion. Partial correction combined with spherical equivalent adjustment can be used as an initial prescription. For example, for an astigmatic prescription of -3.00DC × 180, the initial prescription might be -0.50DS / -2.00DC × 180, and full correction can be introduced gradually after a period of adaptation.
Contact lenses do not cause such image distortion and can provide full correction from the outset.