The cornea and lens are critical components of the eye's refractive media. In a normal eye, the curved cornea and lens refract incoming light from external objects and focus it on the retina at the back of the eyeball, forming a clear optical image. When physiological or pathological factors cause the eye's axial length to become shorter or the refractive power to decrease, parallel light rays entering the eye are refracted by the ocular optical system but converge to a focus behind the retina. This prevents external objects from forming a sharp image on the retina, resulting in hyperopia.
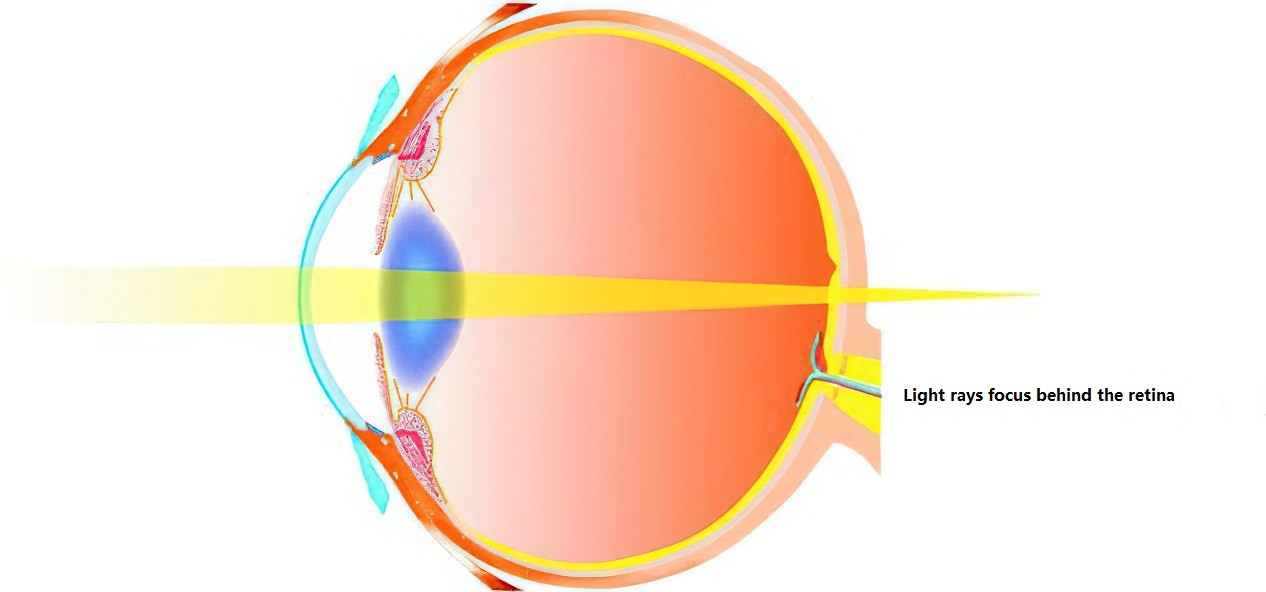
Figure 1 Hyperopic eye
Typical symptoms of hyperopia include blurry distance vision and even blurrier near vision. In cases of mild hyperopia with strong accommodative function, individuals may compensate by using the eye's accommodation to increase refractive power and bring the object into focus on the retina, thereby achieving clear vision. However, excessive use of accommodation may lead to visual fatigue symptoms, especially during near work. For individuals with higher degrees of hyperopia or reduced accommodative capacity due to aging, even additional accommodation cannot produce a clear retinal image. As a result, these individuals may cease to strain their accommodation, leading to less pronounced visual fatigue symptoms but at the expense of overall visual function. Therefore, correcting blurry vision caused by hyperopia in the critical period of visual development is vital for establishing normal visual function.
Etiology and Pathogenesis
In general, newborns exhibit hyperopia due to the immature development of their refractive system, with an average refractive error of +2.50 to +3.00 diopters (D). This type of hyperopia, referred to as physiological hyperopia, typically requires no special treatment. As the eye matures with age, the refractive error gradually decreases, approaching emmetropia.
Congenital abnormalities or acquired factors can result in a refractive error exceeding the range of physiological hyperopia, leading to moderate or high hyperopia. Congenital causes include shortened axial length, small eyeballs, congenital flat corneas, deficient lens refractive power, or aphakia (absence of a lens). Acquired causes include corneal surgeries, corneal trauma, or space-occupying lesions like ocular tumors. Genetic factors play a significant role in the development of high hyperopia, which may present as sporadic cases within families and exhibit autosomal dominant or recessive inheritance patterns. High hyperopia is also associated with conditions like angle-closure glaucoma. Research has indicated that factors such as race, a history of maternal smoking during pregnancy, and a family history of strabismus are linked to an increased risk of developing moderate or high hyperopia.
Classification
Classification by Etiology
Axial Hyperopia
The average axial length of a newborn’s eye is approximately 16 mm. With growth and development during childhood and adolescence, this length increases to 22–24 mm, approaching emmetropia. Environmental or genetic factors may slow eye development or prevent complete emmetropization, potentially halting eye growth and resulting in axial hyperopia. According to ocular refractive calculations, every 1 mm of shortened axial length corresponds to approximately 3 D of hyperopia. Most hyperopic individuals have refractive errors under 6 D; severe high hyperopia is rare and often associated with congenital microphthalmos or ocular maldevelopment. Axial high hyperopia could also result from conditions such as orbital tumors, orbital inflammatory masses, retrobulbar lesions, or retinal detachments.
Curvature Hyperopia
This type of hyperopia results from a decrease in the curvature of the refractive surfaces, particularly the cornea and lens. For instance, an increase in the radius of curvature of the cornea by 1 mm can cause about 6 D of hyperopia. Curvature hyperopia is often accompanied by varying degrees of astigmatism and may stem from congenital flat cornea, corneal trauma, or corneal surgeries.
Refractive Index Hyperopia
This type occurs due to changes in the refractive index of one or more components of the ocular media, resulting in reduced refractive power. Conditions such as age-related cataracts, post-surgical aphakia due to congenital cataracts, or posterior lens dislocation can weaken the lens's refractive power and lead to high hyperopia.
Classification by Degree of Hyperopia
Low Hyperopia (Spherical equivalent ≤ +3.00 D)
In cases of mild hyperopia, strong accommodative function may allow the use of additional accommodation to compensate during distance vision, leading to clear imaging without significant effects on visual acuity or symptoms of visual fatigue.
Moderate Hyperopia (+3.00 D < Spherical Equivalent ≤ +5.00 D)
The additional accommodation may be insufficient for complete compensation. Visual acuity is impaired, accompanied by discomfort and symptoms of visual fatigue. Excessive accommodation efforts may lead to esotropia.
High Hyperopia (Spherical Equivalent > +5.00 D)
High hyperopia results in refractive errors too severe for compensation through accommodation, severely impairing vision and potentially causing refractive amblyopia.
Classification by Accommodative State
Manifest Hyperopia
This refers to the degree of hyperopia measured without cycloplegia (non-cycloplegic refraction), typically under normal pupil conditions. It represents the maximum positive lens power required to achieve emmetropia.
Latent Hyperopia
This is the portion of hyperopia that remains undetected without cycloplegic refraction due to physiological tension of the ciliary muscle.
Total Hyperopia
The total amount of hyperopia, which includes both manifest and latent hyperopia, represents the maximum positive lens power required to fully correct refractive error under cycloplegic conditions.
Absolute Hyperopia
This refers to the portion of hyperopia that cannot be compensated even with full use of accommodation. It is identified as the minimum positive lens power needed to correct refractive error to emmetropia during non-cycloplegic refraction.
Facultative Hyperopia
This is the portion of hyperopia that can be compensated by accommodation. It can be identified during non-cycloplegic refraction and is calculated as the difference between manifest hyperopia and absolute hyperopia.
As patients age, the physiological tension of the ciliary muscle decreases, causing latent hyperopia to gradually become manifest hyperopia. Additionally, the ability and amplitude of accommodation decline, leading facultative hyperopia to become absolute hyperopia. In elderly patients with no accommodative ability, hyperopia becomes entirely manifest, meaning total hyperopia is equal to absolute hyperopia, and facultative hyperopia is zero.
Diagnosis
Age and Patient Complaints
Patients with hyperopia often report symptoms such as reduced visual acuity or eye strain. Some cases of moderate to high hyperopia may also be accompanied by strabismus or amblyopia. The specific visual experiences and symptoms depend largely on both age and the degree of hyperopia.
For patients younger than six years old with mild to moderate hyperopia, strong accommodative ability and minimal near-work demands typically result in the absence of noticeable symptoms. Mild hyperopia is often detected through routine vision screening, while moderate to high hyperopia is often noticed when caregivers observe issues such as esotropia or frequent falls.
In patients aged six to eighteen years (school-age), symptoms begin to emerge due to the increased demand for near work, such as reading. Common complaints include eye strain, orbital pain, difficulty seeing the blackboard, and issues with academic performance.
Between eighteen and forty years of age, patients may complain of visual fatigue symptoms, including sore eyes, eye strain, and headaches, particularly during near work. These symptoms can be temporarily relieved by rest, although some individuals may develop presbyopia earlier than expected.
For individuals older than forty, decreased accommodative function and amplitude result in difficulties with both near and distance vision. Complaints of eye strain and visual fatigue become more pronounced.
Medical and Family History
The diagnosis involves reviewing the onset of symptoms such as reduced visual acuity and visual fatigue, determining whether these symptoms developed gradually or appeared suddenly. The evaluation also considers whether the patient has congenital diseases or developmental abnormalities, a history of corneal trauma or surgery, ocular tumors, retinal pathologies, other systemic conditions, or a family history of hyperopia or related genetic disorders.
Examinations
Visual Acuity Testing
Reduced visual acuity may be observed.
Functional Tests
There may be abnormalities in visual fields, color perception, or stereoscopic vision. Strabismus, such as esotropia or latent esotropia, may also be noted, though ocular motility is generally unaffected.
Slit-Lamp Examination
This test may reveal microphthalmos, a small eyeball, or a relatively shallow anterior chamber.
Refraction Testing
Cycloplegic refraction is recommended.
Fundoscopic Examination
Observations may include signs of pseudo-papillitis, characterized by a smaller, reddened optic disc with unclear borders resembling papilledema or optic neuritis, though long-term fundus observation shows no changes. Genetic testing may aid in diagnosing hereditary high hyperopia, which may include associated fundus changes.
Management
The decision to prescribe corrective lenses for hyperopia depends on the degree of hyperopia, the patient's visual acuity, and the presence of symptoms such as visual fatigue.
In patients with low hyperopia, if visual acuity is normal and there are no symptoms, correction is typically unnecessary. However, if symptoms such as eye strain are present, corrective lenses are required. For cases where visual acuity is not normal or complications are present, correction is necessary.
In children, particularly those with high hyperopia, early correction is essential to prevent refractive amblyopia. Children with hyperopia should undergo cycloplegic refraction, and prescriptions should be based on the results of this examination as well as factors such as age, ocular alignment, and corrected visual acuity. If esotropia or amblyopia is present, the initial prescription should aim for full correction, with adjustments over time based on ocular alignment. In cases where no strabismus or amblyopia is present, physiological hyperopia may be partially accounted for in the prescription, depending on the child’s age.
For adults, hyperopia correction follows the principle of prescribing the highest positive lens power that provides the best corrected visual acuity. Options for correction include eyeglasses, contact lenses (typically rigid gas permeable contact lenses, RGPCL), or refractive surgery.