Etiology
The most common cause of optic chiasmal lesions is pituitary adenomas, followed by tuberculum sellae meningiomas, craniopharyngiomas, anterior communicating artery aneurysms, cavernous sinus tumors, third ventricular tumors or hydrocephalus, optic chiasmal arachnoiditis, optic chiasmal gliomas, clinoid segment artery aneurysms, pituitary apoplexy, and empty sella syndrome, among others.
Clinical Manifestations
A classical sign of optic chiasmal lesions is bitemporal hemianopsia. However, in clinical practice, optic chiasmal damage does not typically manifest as complete bitemporal hemianopsia at the onset but often begins with incomplete quadrantic defects, depending on the location of the chiasmal compression. For instance, pituitary adenomas located below the optic chiasm initially compress the inferonasal fibers of the chiasm, resulting in superior temporal visual field defects. This is followed by defects in the inferior temporal, inferonasal, and superior nasal quadrants. A significant number of pituitary adenoma patients first seek medical attention from ophthalmologists due to visual field defects, and ophthalmologists play a critical role in the early diagnosis of pituitary adenomas.
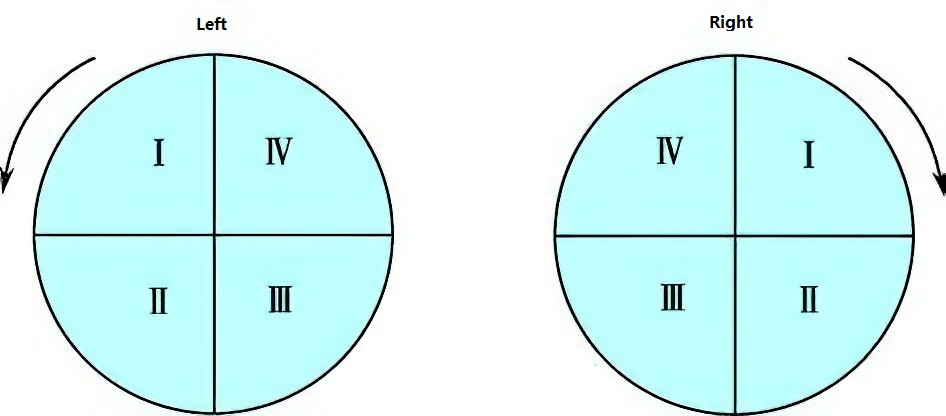
Figure 1 Sequence of visual field defects caused by pituitary adenomas
The arrows indicate that pituitary adenomas located below the optic chiasm initially lead to superior temporal quadrant visual field defects, followed by inferior temporal, inferonasal, and superior nasal quadrant defects.
Tumors originating above the optic chiasm, such as tuberculum sellae meningiomas, craniopharyngiomas, or third ventricular tumors, compress the optic chiasm from top to bottom, resulting in a different sequence of visual field loss. Careful analysis of the pattern of visual field defects in the early stages of the disease helps distinguish between lesions above or below the sella.
In addition to causing the chiasmatic syndrome (comprising visual impairment, visual field defects, and primary optic atrophy), pituitary adenomas can also be associated with endocrine abnormalities, including obesity, hypogonadism, loss of facial hair and erectile dysfunction in males, and menstrual disorders in females. Tumors in the third ventricle causing optic chiasmal lesions are often accompanied by symptoms of raised intracranial pressure, such as headache, vomiting, and papilledema. Craniopharyngiomas, in addition to intracranial hypertension, may show calcified plaques at the tumor site on cranial CT imaging.
Treatment
The primary disease must be treated actively. Early visual field and visual acuity damage caused by optic chiasmal compression from pituitary adenomas can show significant improvement in some patients after surgical resection of the tumor. However, for tumors in the third ventricle or other locations with raised intracranial pressure, secondary optic atrophy resulting from prolonged papilledema often results in poor visual function prognosis.