Optic Nerve Hypoplasia
Optic nerve hypoplasia occurs due to differentiation abnormalities in the retinal ganglion cell layer during the embryonic stage when the embryo measures 13–17 mm. Some studies suggest it may be associated with the use of medications such as phenytoin or quinine during pregnancy.
Fundoscopic Findings
The optic disc appears small and gray, sometimes surrounded by a yellow halo forming a "double-ring sign." Patients often experience reduced visual acuity and visual field abnormalities and may present with microphthalmia, nystagmus, or iris and choroidal colobomas. Systemic manifestations may include pituitary abnormalities, endocrine system issues, or central nervous system defects.
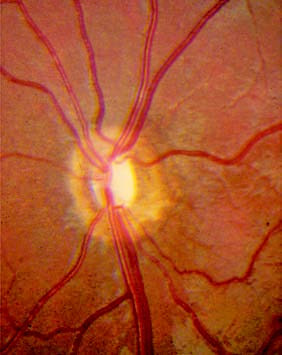
Figure 1 Optic nerve hypoplasia
The optic disc appears small, pale in color, and displays a double-ring sign.
Optic Pit
Optic pits are caused by developmental defects originating in the neuroectoderm, with an incidence of approximately 1 in 11,000. Typically, they affect only one eye. Visual acuity is often preserved unless complicated by macular retinal detachment, which leads to visual deterioration.
Fundoscopic Findings
A round or polygonal pit-like depression is present on the optic disc, with depths as deep as 25 diopters, though typically around 5 diopters. The pit is often covered by gray-white fibroglial tissue and commonly located on the temporal or inferotemporal aspect of the optic disc. The pit may communicate with the subretinal space in the macular region. Among patients aged 20–40, 25–75% develop serous macular disciform retinal detachment, which is a common reason for seeking medical attention. For detachments persisting beyond 3 months with fluid absorption failure and compromised vision, laser photocoagulation is used to seal the communication between the pit and subretinal space. Vitrectomy combined with intraocular photocoagulation may also be employed.

Figure 2 Optic pit
The optic disc shows a pit-like depression located on the temporal side of the disc.
Optic Disc Drusen
Optic disc drusen are non-cellular structures formed by the accumulation of degenerative axoplasmic material from optic nerve fibers. These structures are often calcified and increase in size with age. Some theories suggest they may result from dysplastic proliferation and degeneration of immature glial tissue over the optic disc.
Fundoscopic Findings
The size of optic disc drusen varies. Superficial drusen are easily visible and resemble frog eggs in appearance, with a pale yellow or white, shiny, translucent, or semi-translucent appearance. Deep-seated drusen are covered by glial tissue and may not be visually detectable during fundoscopic examination. Instead, they can create localized elevation with irregular margins mimicking pseudopapilloedema. These are referred to as buried drusen. B-mode ultrasonography can aid in diagnosis, revealing a high-echo structure with posterior acoustic shadows. Visual field testing may show an enlarged physiological blind spot, arcuate defects, or centripetal constriction.

Figure 3 Optic disc drusen
There is an elevation below the optic disc with an uneven surface and a pale yellow coloration.
Optic Disc Coloboma
Optic disc colobomas arise due to incomplete closure of the embryonic fissure. They are often associated with iris or choroidal colobomas and other congenital ocular abnormalities, though isolated optic disc colobomas are less common. The condition typically affects only one eye and is characterized by significant visual impairment.
Fundoscopic Findings
The optic disc appears significantly larger, often several times its normal size. The deficient region appears pale blue with clear margins, forming a large and deep depression. Colobomas are usually located in the inferonasal quadrant or lower half of the optic disc. Blood vessels emerge from the margins of the coloboma and exhibit a hook-like curvature. Visual field testing reveals an enlarged physiological blind spot.

Figure 4 Optic disc coloboma
The optic disc is significantly larger, several times the normal size. The defect area appears pale blue with sharp margins, forming a large and deep depression located in the inferonasal portion of the disc.
Morning Glory Syndrome
Morning glory syndrome is believed to result from incomplete closure of the upper portion of the embryonic fissure or mesodermal abnormalities. It represents a unique type of optic disc developmental anomaly.
Fundoscopic Findings
The optic disc appears funnel-shaped and enlarged, measuring 3–5 times its normal size. Surrounding the disc are pink peripheral regions, while its base is filled with white wool-like tissue. Blood vessels exhibit radial distribution, with arteries and veins indistinct from one another. Pigment rings and atrophic areas surround the optic disc. Patients may present with other congenital ocular abnormalities or intracranial vascular malformations. Magnetic resonance angiography (MRA) is recommended for further evaluation.

Figure 5 Morning glory syndrome
The optic disc resembles a blooming morning glory flower, appearing 3–5 times larger than a normal disc. It is funnel-shaped, with pink coloration at the periphery and the base filled with white wool-like tissue.