Optic disc edema, also known as papilledema, refers to a swelling and elevation of the optic disc. The three layers of the optic nerve sheath are continuous with the three layers of the intracranial meninges. Raised intracranial pressure (ICP) can be transmitted to the optic nerve through the cerebrospinal fluid. Under normal conditions, intraocular pressure is higher than intracranial pressure, but disruption of this balance can result in optic disc edema.
Etiology
Optic disc edema can be classified into non-inflammatory and inflammatory causes. The most common reasons include elevated intracranial pressure due to intracranial tumors, inflammation, trauma, or congenital anomalies, as well as benign intracranial hypertension. Other causes include systemic conditions such as hypertensive crises, nephritis, severe anemia, hematologic disorders, emphysema, and certain cases of right heart failure, as well as high-altitude illness. Orbital space-occupying lesions (causing compressive optic neuropathy) and ocular conditions such as optic neuritis, neuroretinitis, central retinal vein occlusion, primary or metastatic optic nerve tumors, uveitis, and persistent hypotony after ocular trauma or surgery can also cause optic disc edema. Focus is placed here on optic disc edema caused by elevated intracranial pressure.
Clinical Features
In early stages, visual acuity is often normal, though transient episodes of visual blurring may occur. Symptoms such as headache, diplopia, nausea, and vomiting may be present. Visual loss is rare but can occur in acute or severe chronic cases, typically accompanied by visual field defects.
Fundoscopic Findings
In the early stages, optic disc edema may be asymmetrical, with the disc margins appearing blurred and often obscuring blood vessels. Swelling of the nerve fiber layer is common. Notably, if one eye has optic atrophy or hypoplasia, optic disc edema does not develop in that eye, and thus unilateral optic disc edema may be observed clinically.
Optic disc edema can be classified into four stages:
- Early stage: The optic disc appears hyperemic, with small superficial hemorrhages near the optic disc margin. The blurred disc margins often follow a progression from the inferior, superior, nasal, to temporal regions, corresponding to varying nerve fiber thickness.
- Progressive stage: Bilateral optic disc edema becomes pronounced, often with flame-shaped hemorrhages and cotton-wool spots indicative of nerve fiber infarction. Macular star exudates or hemorrhages may also occur.
- Chronic stage: The optic disc shows a rounded elevation, with the optic cup disappearing. Shiny hard exudates suggest that the swelling has persisted for months.
- Atrophic stage: The optic disc becomes pale gray, retinal vessels become narrowed and sheathed, and vascular shunting on the disc may develop. Pigment epithelial changes in the peripapillary and macular regions may be seen.
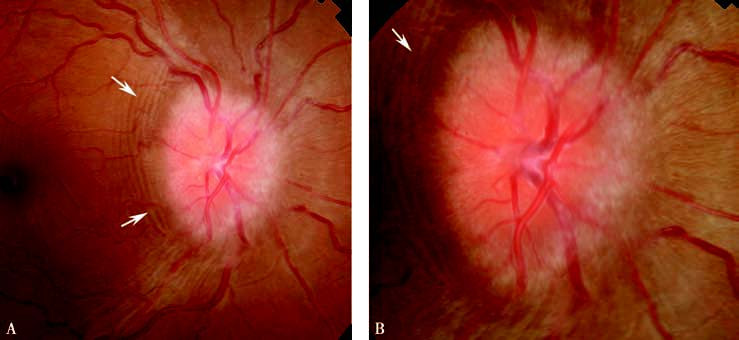
Figure 1 Optic disc edema
A progressive edema of the optic disc is shown, accompanied by choroidal folds (indicated by arrows).
A and B: Low and high magnification views.
Visual Field Testing
Enlargement of the physiological blind spot with normal peripheral visual fields is common. Severe optic disc edema or progression to optic atrophy can lead to significant central visual loss and reduction of peripheral fields, particularly in the inferior nasal region.
Diagnosis
Typical cases of optic disc edema are relatively easy to diagnose clinically. Determining the cause often requires further examination, including CT or MRI of the head and orbit or consultation with neurology. If CT and MRI are inconclusive, lumbar puncture may be necessary. Additional tests may be considered for thyroid-related disorders, diabetes, and anemia.
Differential Diagnosis
Pseudopapilledema
This is often associated with optic disc drusen. The disc tends to be small and non-hyperemic, with vessels not obscured. Spontaneous retinal venous pulsation is often present. B-scan ultrasound typically reveals buried optic disc drusen.
Optic Disc Inflammation
This condition lacks symptoms of increased ICP and presents with significant visual impairment and color vision loss. Pain with eye movement may be present. Optic disc elevation usually does not exceed 3 diopters, and hemorrhages or exudates are uncommon.
Optic Disc Vasculitis: Common in healthy individuals under 40 and typically affects one eye. Patients usually experience painless visual blurring with mild or normal visual acuity. The optic disc appears markedly hyperemic and swollen, with peripapillary hemorrhages and exudates. Retinal veins appear dilated and tortuous, while arteries remain unchanged. FFA reveals delayed venous filling and fluorescein leakage from capillaries and retinal vein walls. The prognosis is generally good, with high-dose corticosteroid therapy being effective.
Anterior Ischemic Optic Neuropathy (AION)
This disease presents with mild disc edema, typically unilateral and with a sudden onset. Classic visual field defects are often seen.
Leber Hereditary Optic Neuropathy (LHON)
This commonly occurs in males aged 10–30. Initially unilateral but quickly progresses to bilateral involvement. Rapid vision loss is accompanied by optic disc hyperemia and peripapillary capillary telangiectasia. FFA shows no fluorescein leakage from the disc. Field defects are usually central scotomata.
Treatment
Treatment focuses on addressing the underlying cause.