Retinoschisis refers to the splitting of the layers within the retinal neurosensory tissue. Congenital X-linked retinoschisis (XLRS), also known as juvenile retinoschisis, is a hereditary condition primarily seen in children and young adults, caused by mutations in the RS1 gene. Pathological studies have demonstrated that peripheral schisis most commonly occurs between the outer plexiform layer and the nerve fiber layer. It is often identified in patients presenting with strabismus, nystagmus, or poor vision, but may also be discovered during examinations performed for vitreous hemorrhage.
Clinical Features
Patient Population and Visual Function
The disease primarily affects males, with both eyes being involved, though the severity may be asymmetric. Visual acuity typically ranges from 0.1 to 0.5.
Fundus Findings
In the early stages, the foveal reflex disappears. With disease progression, the macula may develop radiating cystic folds centered around the fovea, with the classic presentation resembling a "spoke-wheel pattern." Approximately 50% of patients exhibit peripheral retinal schisis, most commonly in the inferotemporal quadrant. This appears as a flat, large schisis cavity, with the inner wall of the schisis being thin like a veil and often accompanied by an inner layer retinal break. If both the inner and outer layers develop breaks in the schisis cavity, retinal detachment may occur. Hemorrhage into the vitreous is frequently observed if retinal blood vessels within the schisis are torn.
Diagnosis
Electrophysiology Testing
Electroretinography (ERG) reveals a characteristic "negative waveform," where the b-wave amplitude is reduced, appearing inverted compared to the a-wave, which remains normal or near normal.
Optical Coherence Tomography (OCT)
Imaging shows retinal separation in the macular region, characterized by evenly spaced bridging structures connecting the layers.
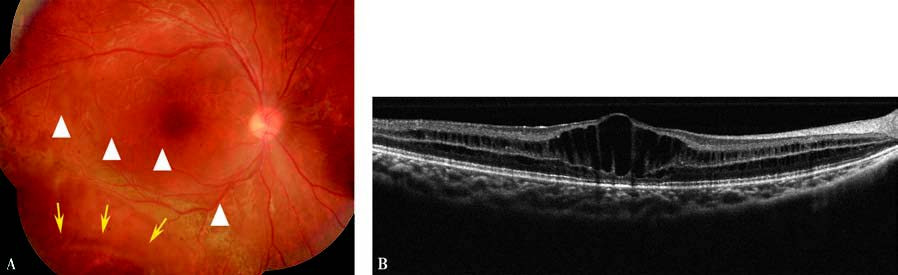
Figure 1 Right eye with X-linked retinoschisis.
A. Fundus photograph displays radiating cystic folds in the macular region, accompanied by peripheral schisis in the inferotemporal quadrant (yellow arrow) and an inner layer retinal break within the schisis cavity (white triangle).
B. OCT image shows separation between retinal layers in the macular region, with characteristic bridging structures.
A/B-Scan Ultrasound
Peripheral schisis can be identified, which also aids in differentiating retinoschisis from retinal detachment.
Family History and Genetic Testing
A positive family history combined with genetic testing for RS1 mutations can provide confirmation of the diagnosis.
Treatment
The disease is often stable in most patients, and spontaneous improvement in fundus abnormalities may occur in some cases. Close monitoring is essential. When peripheral lesions extend to the macula and significantly impair vision, or in cases involving recurrent vitreous hemorrhage or retinal detachment, prompt intervention such as vitrectomy, laser photocoagulation, or cryotherapy, alone or in combination, is recommended. Gene therapy for XLRS is currently under investigation.